DOP19 Urinary metabolome in newly diagnosed treatment-naïve Crohn’s Disease patients: Results from the IBDomics study
Aldars-García, L.(1);Gil-Redondo, R.(2);Embade, N.(2);Riestra, S.(3);Rivero, M.(4);Gutiérrez, A.(5);Rodríguez, I.(6);Fernández, L.(7);Ceballos, D.(8);Benítez, J.M.(9);Aguas, M.(10);Bastón-Rey, I.(11);Algaba, A.(12);Casanova, M.J.(1);Lorente, R.(13);Ber, Y.(14);Royo, V.(15);Esteve, M.(16);Millet, O.(2);Gisbert, J.P.(1);Chaparro, M.(1);
(1)Hospital Universitario de La Princesa IIS-P and CIBERehd, Gastroenterology, Madrid, Spain;(2)CIC bioGUNE, Precision Medicine and Metabolism Lab, Derio, Spain;(3)Hospital Universitario Central de Asturias, Gastroenterology, Asturias, Spain;(4)Hospital Universitario Marqués de Valdecilla and IDIVAL, Gastroenterology, Santander, Spain;(5)Hospital General Universitario de Alicante- CIBERehd and Instituto de Investigación Sanitaria y Biomédica de Alicante ISABIAL, Gastroenterology, Alicante, Spain;(6)Hospital Galdakao-Usansolo, Gastroenterology, Vizcaya, Spain;(7)Hospital Clínico Universitario de Valladolid, Gastroenterology, Valladolid, Spain;(8)Universitario de Gran Canaria Dr. Negrín, Gastroenterlogy, Las Palmas de Gran Canaria, Spain;(9)Hospital Universitario Reina Sofía and IMIBIC, Gastroenterology, Córdoba, Spain;(10)Hospital Universitari i Politecnic La Fe and CIBERehd, Gastroenterology, Valencia, Spain;(11)Complexo Hospitalario Universitario de Santiago, Gastroenterology, Santiago de Compostela, Spain;(12)Hospital Universitario de Fuenlabrada e Instituto de Investigación Hospital Universitario La Paz IdiPAZ, Gastroenterology, Madrid, Spain;(13)Hospital General Universitario de Ciudad Real, Gastroenterology, Ciudad Real, Spain;(14)Hospital San Jorge, Gastroenterology, Huesca, Spain;(15)Hospital Universitari Son Espases, Gastroenterology, Palma de Mallorca, Spain;(16)Hospital Universitari Mutua Terrasa, Gastroenterology, Terrasa, Spain
Background
The urinary metabolome of patients with Crohn’s disease (CD) differs significantly from healthy subjects and, among other features, reflects the specific gut dysbiosis affecting these patients. However, most of the studies included established and treated CD patients. Our aim was to characterize the urinary metabolome of onset and treatment-naïve CD patients and to identify the metabolic profile related to the different CD clinical classifications.
Methods
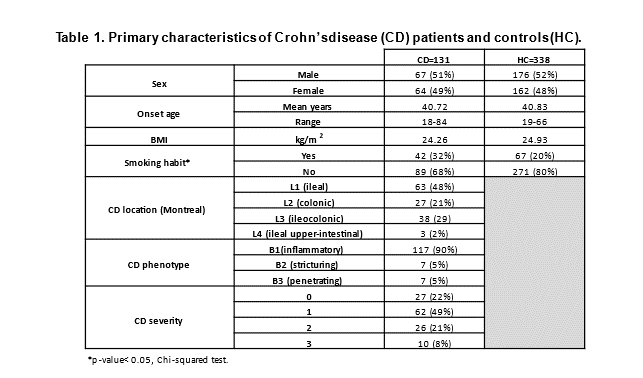
Patients newly diagnosed with CD (n=131) were prospectively included. Control healthy subjects (HC, n=338) were recruited among the general population and matched for sex, age and BMI to the IBD subjects. Fasting urine was obtained before starting any treatment. Metabolomic analysis was performed by proton nuclear magnetic resonance (1H NMR).
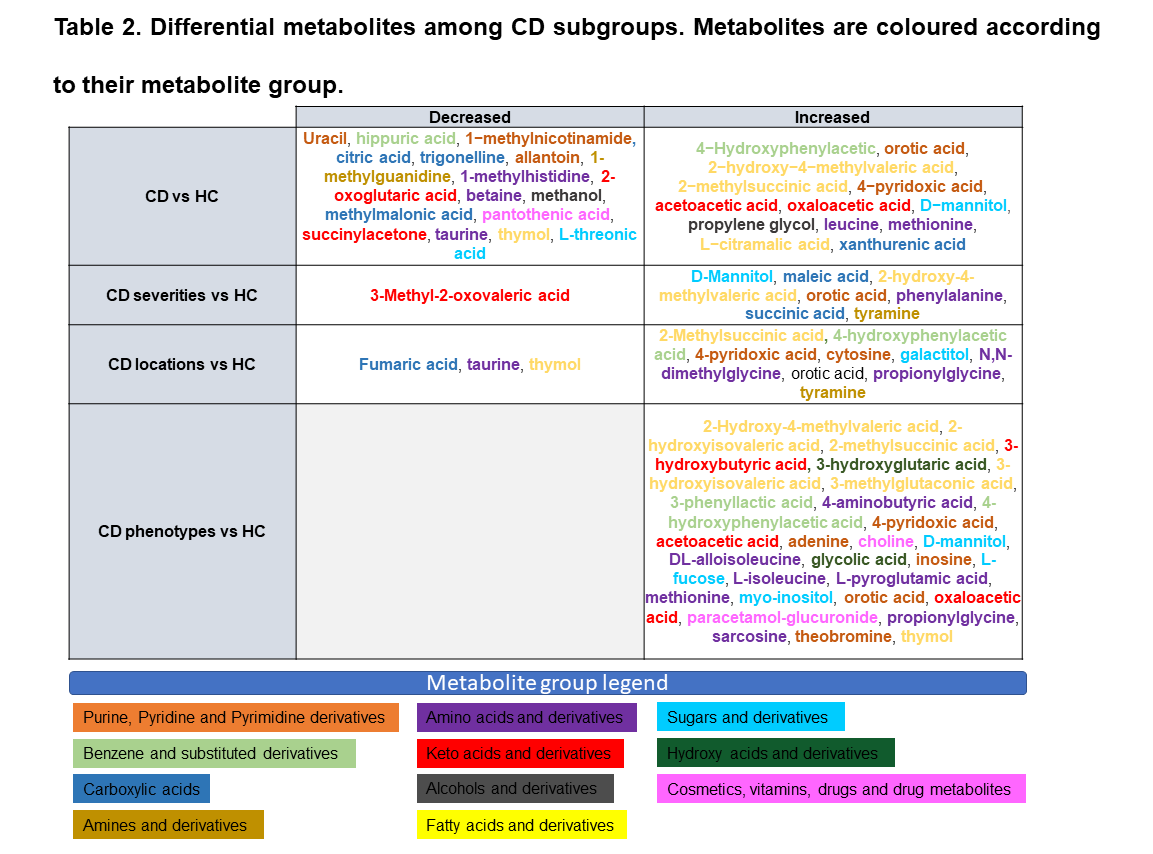
We performed a comparative assessment of the urinary metabolome profile using a linear regression model for each metabolite, including sex, age, BMI, and smoking habit as covariates to control for confounding. The different subgroup comparisons within CD were made as follows: (1) CD; (2) CD location (Montreal Classification): L1 (ileal) + L4 (ileal and upper-intestinal), L2 (colonic) and L3 (ileocolonic); (3) endoscopic CD activity: 0, 1, 2 and 3; and (4) CD phenotype: B1 (inflammatory), B2 (stricturing) and B3 (penetrating), versus HC. In addition, data analysis was carried out using partial least squares-discriminate analysis (PLS-DA) to determine class membership based on distinct metabolomic profile.
Results
The primary characteristics of the CD patients and HC are shown in Table 1. Several metabolites were identified to be differently abundant in each group (Table 2). These metabolites are involved in relevant processes related to energy and aminoacids metabolism, and also include gut-derived metabolites. The PLS-DA model separated patients within the different clinical subgroups (Figures 1-4). Figures 1-4(b) show the main metabolites involved in each group separation. Many of these metabolites are in accordance with the differential metabolites obtained using the univariate analysis (Table 2), showing the potential of this approach to group CD patients and to identify potential biomarkers.


Conclusion
Analysis of urinary metabolites can help to understand the etiopathological mechanisms in CD. It has the potential to provide a non-invasive means of diagnosing CD, and can differentiate between CD clinical expressions.
- Posted in: DOP Session 3 - New biomarkers


