N09 Exploration of medication adherence interventions in Inflammatory Bowel Disease, Multiple Sclerosis and Rheumatoid Arthritis: A Scoping Review of Randomised Controlled Trials.
King, K.(1)*;McGuinness, S.(1);Watson, N.(1);Norton, C.(1);Chalder, T.(2);Czuber-Dochan, W.(1);
(1)King's College London, Faculty of Nursing- Midwifery & Palliative Care, London, United Kingdom;(2)King's College London, Institute of Psychiatry- Psychology and Neuroscience, London, United Kingdom; Bowel Research in Nursing Group
Background
The inflammatory diseases of inflammatory bowel disease (IBD), multiple sclerosis (MS) and rheumatoid arthritis (RA) have recognised medications to maintain remission.Yet between 53–75% of people with IBD, 30-80% with RA and up to 50% with MS do not take medications as prescribed.
Recognising and improving adherence in IBD, MS and RA is a primary treatment goal to keep symptoms quiescent.
This scoping review aims to identify effective adherence interventions for IBD, MS and RA. As there were few studies in IBD, MS and RA were included to learn lessons from other conditions.
Methods
Randomised controlled trial (RCT) medication adherence interventions for IBD, MS or RA conducted between 2012-2021, were identified in six electronic databases.
Critical Appraisal Skills Programme assessed study quality.
Results
3024 participants were included across 24 RCTs; 8(33.3%) investigating IBD, 12(50%) RA and 4(16.7%) MS.
Nine RCTs (37.5%) significantly improved medication adherence; all were rated high quality with five being delivered face to face and 1:1; all involving tailored education, advice or counselling by trained health professionals (HPs).
IBD interventions were varied; the two significantly effective were web-based; one offering education modules and “red flag” monitoring, with follow up testing versus telephone education. The other used text message reminders with tailored feedback.
Four of five effective RA interventions used psychological, behaviour change approaches.Three integrated educational and artificial intelligence-based methods through telephone-education, viewing disease progression on a computer system or text messages.
Of the four MS interventions, only a Bluetooth bottle cap with mobile phone reminders and MI based telephone counselling led to significant adherence improvements.
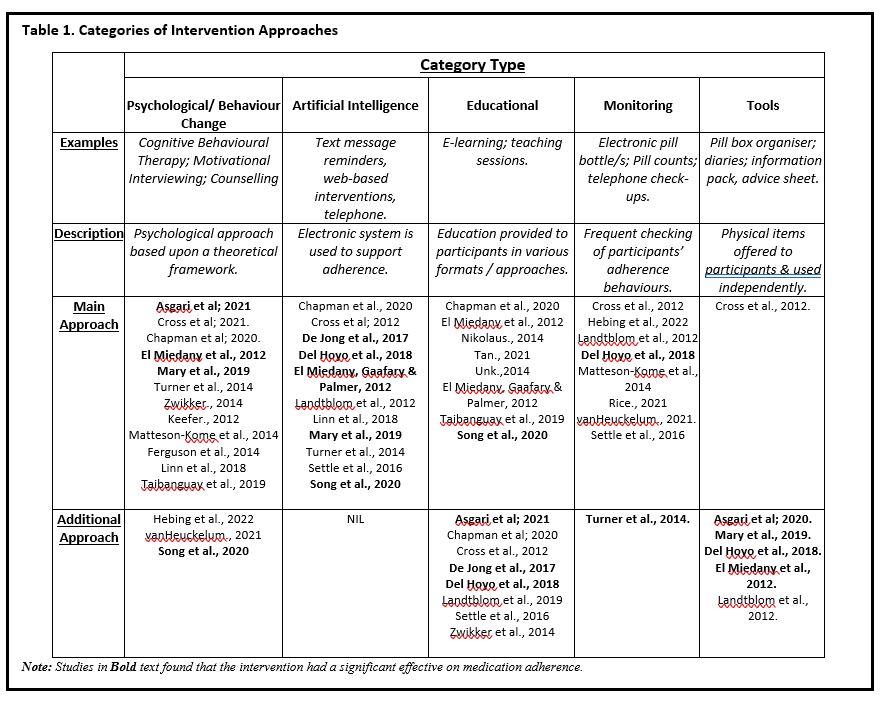
Interventions using artificial intelligence were most significantly effective (see Table 1). Tools such as diaries, calendars and advice sheets were also effective in increasing adherence.
Only 10 interventions were theory based.
Conclusion
Tailored, face to face, 1:1 interaction with HPs can provide personalised, adherence support.
Integration of several therapeutic approaches can be effective, but it can be difficult to identify cause of any impact.
To improve adherence in inflammatory conditions, theoretically informed interventions should be developed and evaluated.
Online routes of intervention delivery must be accessible, user-friendly, and functional to promote self-management.
However, an adherence intervention which minimises costs, provides patient-centred, value-based care through implementation of evidence-based strategies will no doubt be welcomed by patients, HPs and services alike.