OP10 Proctocolectomy with permanent ileostomy is associated with better transplant-free survival in patients with primary sclerosing cholangitis: a retrospective cohort study
Mol, B.(1)*;van Nieuwamerongen, M.(1);van Munster, K.(1);van Munster, S.(1);de Vries, A.(2);van der Meer, A.(2);Goet, J.(2);Weersma, R.(3);Inderson, A.(4);Boonstra, K.(1);van Meer, S.(5);de Boer, Y.(1);Spanier, M.(6);Drenth, J.(7);de Vries, E.(8);Beuers, U.(1);Bogaards, J.(9);Ponsioen, C.(1);
(1)Amsterdam UMC, Gastroenterology and Hepatology, Amsterdam, The Netherlands;(2)Erasmus MC, Gastroenterology and Hepatology, Rotterdam, The Netherlands;(3)University Medical Centre Groningen, Gastroenterology and Hepatology, Groningen, The Netherlands;(4)Leiden University Medical Centre, Gastroenterology and Hepatology, Leiden, The Netherlands;(5)University Medical Centre Utrecht, Gastroenterology and Hepatology, Utrecht, The Netherlands;(6)Rijnstate Hospital, Gastroenterology and Hepatology, Arnhem, The Netherlands;(7)Radboud University Medical Centre, Gastroenterology and Hepatology, Nijmegen, The Netherlands;(8)Isala Hospital, Gastroenterology and Hepatology, Zwolle, The Netherlands;(9)Amsterdam UMC, Epidemiology and Data Science, Amsterdam, The Netherlands; EpiPSC2
Background
Inflammatory bowel disease (IBD) is the strongest known risk factor for primary sclerosing cholangitis (PSC) and seems associated with a worse prognosis. After liver transplantation, colectomy is associated with decreased rates of recurrent PSC and better graft survival.1 At the same time, the effect of colectomy on the disease course of PSC remains unclear.2 Available evidence depends either on small patient numbers, may be confounded by unobserved risk factors or colectomy was not considered as time-depending covariate. The aim of our study is to estimate the effect of colectomy on the disease course of PSC by taking time dependency and known risk factors into account.
Methods
We conducted a retrospective cohort study between January 1st 2008 and December 31st 2021 based on the Dutch population-based EpiPSC2 cohort. Transplant-free survival was defined as liver transplantation or PSC-related death (excluding colorectal carcinoma). The effect of colectomy was determined as time depending variable via Cox proportional hazards regression and was corrected for the following known risk factors; sex, age at diagnosis, large or small duct PSC, features of auto-immune hepatitis, time depending IBD status (i.e. no IBD, ulcerative colitis (UC), Crohn’s disease (CD) or IBD Unspecified (IBD-U)), and tertiary centre inclusion.
Effect of colectomy was stratified for extent (i.e. hemi-, subtotal, or proctocolectomy with pouch or ileostomy). Indication of colectomy (i.e. active disease, dysplasia and colorectal carcinoma or other) was also considered as predictor variable. Events in the first year after colectomy were censored due to a presumed delayed effect of colectomy on disease course.
Results
Of the 1341 patients included, 912(68%) were diagnosed with IBD and 187(14%) had undergone a colectomy. During a total follow-up of 14,393 patient years, 370(28%) patients underwent liver transplantation and 318(24%) patients died due to a PSC-related cause. Median transplant-free survival time was 20 years. Hazard ratio (HR) was significantly decreased in patients who had undergone proctocolectomy with ileostomy (HR 0.47(0.24-0.93)) compared to patients without colectomy. This effect was absent in the group with any other type of colectomy (HR 0.90(0.67-1.19)). Indication of colectomy had no apparent effect. Presence of UC, CD or IBD-U was not associated with a worse prognosis compared to absence of IBD (HR 0.99(0.81-1.21), HR 0.85(0.64-1.13), HR 0.75(0.43-1.29)).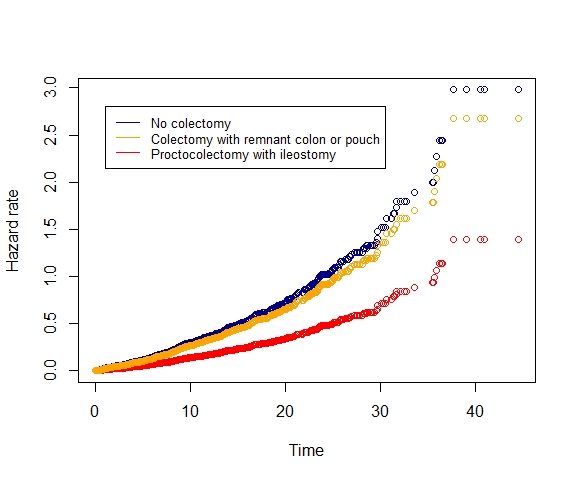
Conclusion
Our data suggest that proctocolectomy with ileostomy confers protection for liver transplantation and PSC-related death. This points towards the putative pathophysiologic role of the colonic microbiota in PSC and may open avenues to a better understanding of the aetiology of PSC.


