OP20 Risk and predictors of surgery in a newly diagnosed cohort of IBD patients in the biologic era: Results from the EpidemIBD study
Chaparro, M.(1);Garre, A.(1);Núñez Ortiz , A.(2);Diz-Lois Palomares, M.T.(3);Rodríguez, C.(4);Riestra, S.(5);Vela, M.(6); Benítez, J.M.(7);Fernández Salgado, E.(8);Sánchez Rodríguez, E.(9);Hernández, V.(10);Ferreiro-Iglesias, R.(11);Ponferrada Díaz, Á.(12);Barrio, J.(13); Huguet, J.M.(14);Arias, L.(15);Martín-Arranz, M.D.(16);Calvet, X.(17);Ginard, D.(18);Alonso-Abreu, I.(19);Fernández-Salazar, L.(20);Varela Trastoy, P.(21);Rivero, M.(22);Vera-Mendoza, I.(23);Vega, P.(24);Navarro, P.(25);Sierra, M.(26); Cabriada, J.L.(27);Aguas, M.(28);Vicente, R.(29);Navarro-Llavat, M.(30);Echarri, A.(31);Gomollón, F.(32);Guerra del Río, E.(33);Casanova, M.J.(1);Spicakova, K.(34);Ortiz de Zarate, J.(35);Alonso-Galán, H.(36);Barreiro-de Acosta, M.(11);Gisbert, J.P.(1)
(1)Hospital Universitario de La Princesa- Instituto de Investigación Sanitaria Princesa IIS-IP- Universidad Autónoma de Madrid- and Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas CIBERehd, Gastroenterology Unit, Madrid, Spain;(2)Hospital Universitario Virgen del Rocío, Gastroenterology Unit, Sevilla, Spain;(3)Hospital Universitario A Coruña, Gastroenterology Unit, A Coruña, Spain;(4)Complejo Hospitalario de Navarra, Gastroenterology Unit, Pamplona, Spain;(5)Hospital Universitario Central de Asturias and ISPA, Gastroenterology Unit, Oviedo, Spain;(6)Complejo Hospitalario Universitario Ntra. Sra. de Candelaria, Gastroenterology Unit, Santa Cruz de Tenerife, Spain;(7)Hospital Universitario Reina Sofía and IMIBIC, Gastroenterology Unit, Córdoba, Spain;(8)Complexo Hospitalario Universitario de Pontevedra- Instituto de Investigación Sanitaria Galicia Sur, Gastroenterology Unit, Pontevedra, Spain;(9)Hospital Ramón y Cajal, Gastroenterology Unit, Madrid, Spain;(10)Hospital Álvaro Cunqueiro. Estrutura Organizativa de Xestión Integrada de Vigo, Gastroenterology Unit, Vigo, Spain;(11)Complexo Hospitalario Universitario de Santiago, Gastroenterology Unit, Santiago de Compostela, Spain;(12)Hospital Universitario Infanta Leonor, Gastroenterology Unit, Madrid, Spain;(13)Hospital Universitario Rio Hortega, Gastroenterology Unit, Valladolid, Spain;(14)Consorcio Hospital General Universitario de Valencia, Gastroenterology Unit, Valencia, Spain;(15)Hospital Universitario de Burgos, Gastroenterology Unit, Burgos, Spain;(16)Hospital Universitario La Paz- School of Medicine. Universidad Autónoma de Madrid. Hospital La Paz Institute for Health Research- La Paz Hospital, Gastroenterology Unit, Madrid, Spain;(17)Hospital Universitari Parc Taulí- Sabadell. Departament de Medicina- Universitat Autònoma de Barcelona. CIBERehd - Instituto de Salud Carlos III, Gastroenterology Unit, Barcelona, Spain;(18)Hospital Universitari Son Espases, Gastroenterology Unit, Palma de Mallorca, Spain;(19)Hospital Universitario de Canarias H.U.C, Gastroenterology Unit, Santa Cruz de Tenerife, Spain;(20)Hospital Clínico Universitario de Valladolid, Gastroenterology Unit, Valladolid, Spain;(21)Hospital de Cabueñes, Gastroenterology Unit, Gijón, Spain;(22)Hospital Universitario Marqués de Valdecilla and IDIVAL, Gastroenterology Unit, Santander, Spain;(23)Hospital Universitario Puerta de Hierro Majadahonda, Gastroenterology Unit, Madrid, Spain;(24)Complexo Hospitalario Universitario de Ourense, Gastroenterology Unit, Ourense, Spain;(25)Hospital Clínico Universitario de Valencia- Universitat de València, Gastroenterology Unit, Valencia, Spain;(26)Complejo Asistencial Universitario de León, Gastroenterology Unit, León, Spain;(27)Hospital de Galdakao-Usansolo, Gastroenterology Unit, Galdakao, Spain;(28)Hospital Universitari i Politecnic La Fe and CIBERehd, Gastroenterology Unit, Valencia, Spain;(29)Hospital Universitario Miguel Servet, Gastroenterology Unit, Zaragoza, Spain;(30)Hospital de Sant Joan Despí Moisès Broggi, Gastroenterology Unit, Barcelona, Spain;(31)Complejo Hospitalario Universitario de Ferrol, Gastroenterology Unit, A Coruña, Spain;(32)Hospital Clínico Universitario “Lozano Blesa”- IIS Aragón and CIBERehd, Gastroenterology Unit, Zaragoza, Spain;(33)Hospital Universitario de Gran Canaria Dr. Negrín, Gastroenterology Unit, Las Palmas, Spain;(34)Hospital Universitario de Araba sede Txagorritxu y sede Santiago, Gastroenterology Unit, Álava, Spain;(35)Hospital Universitario de Basurto, Gastroenterology Unit, Bilbao, Spain;(36)Hospital Universitario Donostia-Donostia Unibertsitate Ospitalea- Guipuzkoa and Organizacion Sanitaria Integrada Tolosaldea- Clínica Santa María de la Asunción, Gastroenterology Unit, Guipúzcoa, Spain On behalf of EpidemIBD Study Group
Background
The management of inflammatory bowel disease (IBD) has substantially changed in the last decades, both in relation to medical and surgical treatments.
Aims: Principal: To know the rate of surgery in a newly diagnosed IBD cohort within the first year after diagnosis. Secondary: To describe the type of surgeries and indications in this cohort, and to identify predictive factors for surgery (focused on intestinal resection) in these patients.
Methods
Prospective, population-based nationwide registry. Adult patients diagnosed with IBD -Crohn’s disease (CD) and ulcerative colitis (UC)- during 2017 in Spain were included and were followed-up for 1 year. Kaplan-Meier curves were used to calculate the rate of surgery. In patients with intestinal resections, only medical treatments before surgery were considered. Predictive factors for surgery were identified by Cox-regression analysis.
Results
3,454 patients (1,647 CD and 1,807 UC) were included (table 1).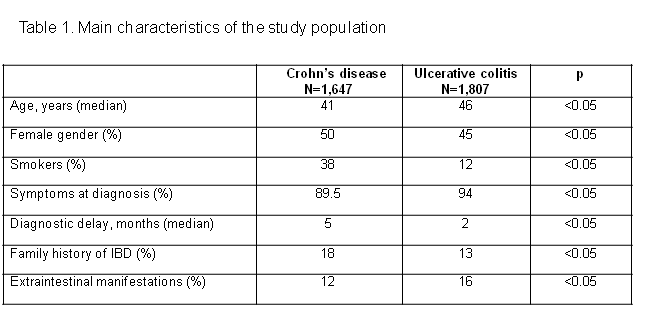
The incidence rate for surgery was significantly higher among CD patients (figure 1).
A total of 197 patients (6%) underwent surgery within the first 12 months: 126 (64%) intestinal resections, and 71 (36%) perianal surgeries. Fifty-seven percent of intestinal resections were urgent, and 43% elective. The main indications for intestinal resections were: intestinal obstruction in 37%, abscess/fistula in 27%, perforation/acute abdomen in 25%, and refractoriness to medical treatment in 18% of cases. A total of 174 CD patients (10.6%) underwent surgery ¾61% intestinal resections and 39% perianal. Twenty-three UC patients (1.3%) were operated on; the number of surgeries in UC was too low to identify predictive factors. In CD patients, to have been treated with thiopurines [Hazard ratio (HR)=0.2, 95% confidence interval (CI)=0.1-0.3) was associated with lower likelihood of intestinal resection. Disease behaviour at diagnosis [stricturing vs. inflammatory (HR=6.5, 95%CI=4-10) and fistulising vs. inflammatory (HR=13, 95%CI=9-21)] was associated with the risk of intestinal resection. Biologic treatment was not associated with the likelihood of intestinal resection (figure 2).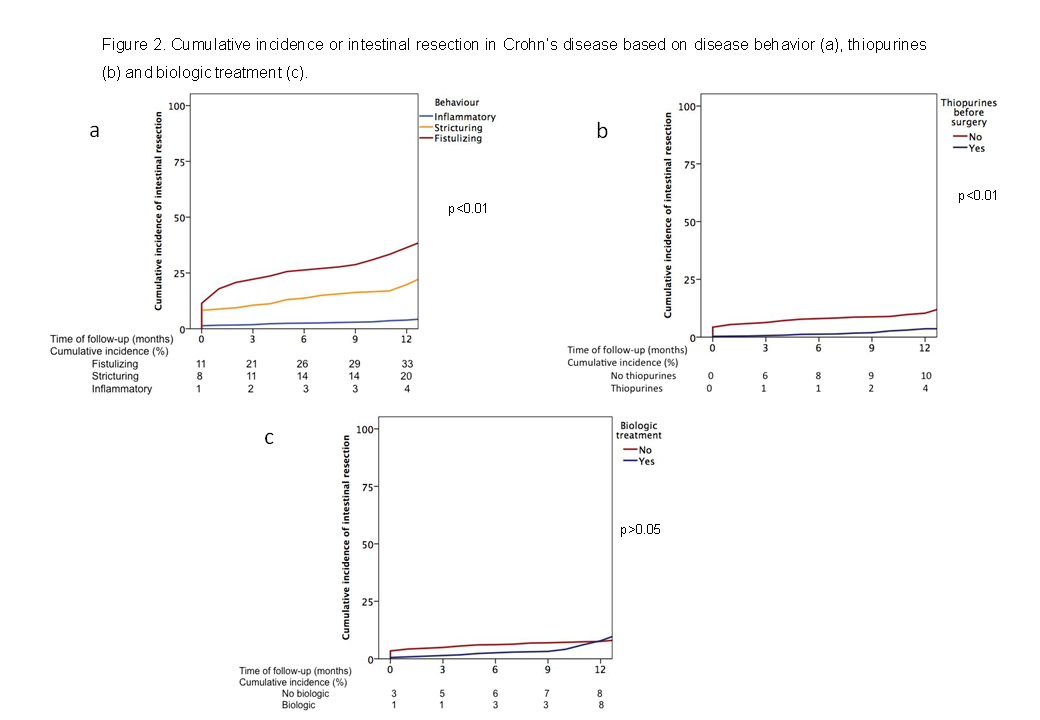
Conclusion
Six percent of IBD patients undergo surgery within the first year of diagnosis, being higher in CD (11%) than in UC (1.3%). Sixty percent of intestinal resections are urgent procedures. The risk of surgery is increased in CD patients with fistulising and stricturing behaviour. Thiopurine, but not biologic treatment, is associated with lower risk of surgery.


