P058 Immunological effects of hepatitis B virus vaccination in inflammatory bowel disease patients
Soleto, I.(1)*;C. Marin, A.(1);Mora, I.(1);Villagrasa, J.R.(2);Baldan-Martin, M.(1);Ramírez, C.(1);Bernardo, D.(3);Chaparro, M.(1);P. Gisbert, J.(1);
(1)Hospital Universitario de La Princesa- Instituto de Investigación Sanitaria Princesa IIS-Princesa- Universidad Autónoma de Madrid UAM- and Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas CIBERehd- Madrid. Spain, gastrointestinal unit, Madrid, Spain;(2)Hospital Universitario de La Princesa, Unidad de medicina preventiva, Madrid, Spain;(3)Mucosal Immunology Lab- instituto de Biología y Genética Molecular IBGM- Universidad de Valladolid-CISC- Valladolid- Spain, Mucosal Immunology Lab, Valladolid, Spain;
Background
The response rate to hepatitis B virus (HBV) vaccination in the general population is about 90%. However, the response rate to the vaccine in patients with inflammatory bowel disease (IBD) is significantly lower. IBD is a multifactorial disease so, it is important to study which cell subsets are involved in the failure of the HBV vaccine. Therefore, our main objective was to study the differences between the circulating immune system of responders and not responders to the vaccine.
Methods
Observational clinical practice study on the factors associated with the immunogenicity of the HBV vaccine in patients with IBD. Per clinical practice, 19 IBD patients vaccinated for the first time against HBV were included. Patients were divided according to their vaccination response after three doses of the vaccine at 0, 1, and 6 months as responders (≥ 100 anti-HBV) and non-responders (< 100 anti-HBV). Blood was collected before and after vaccination to characterize the different immune subsets by flow cytometry. Data were analyzed manually and by high dimensional data analysis (UMAP and FlowSOM).
Results
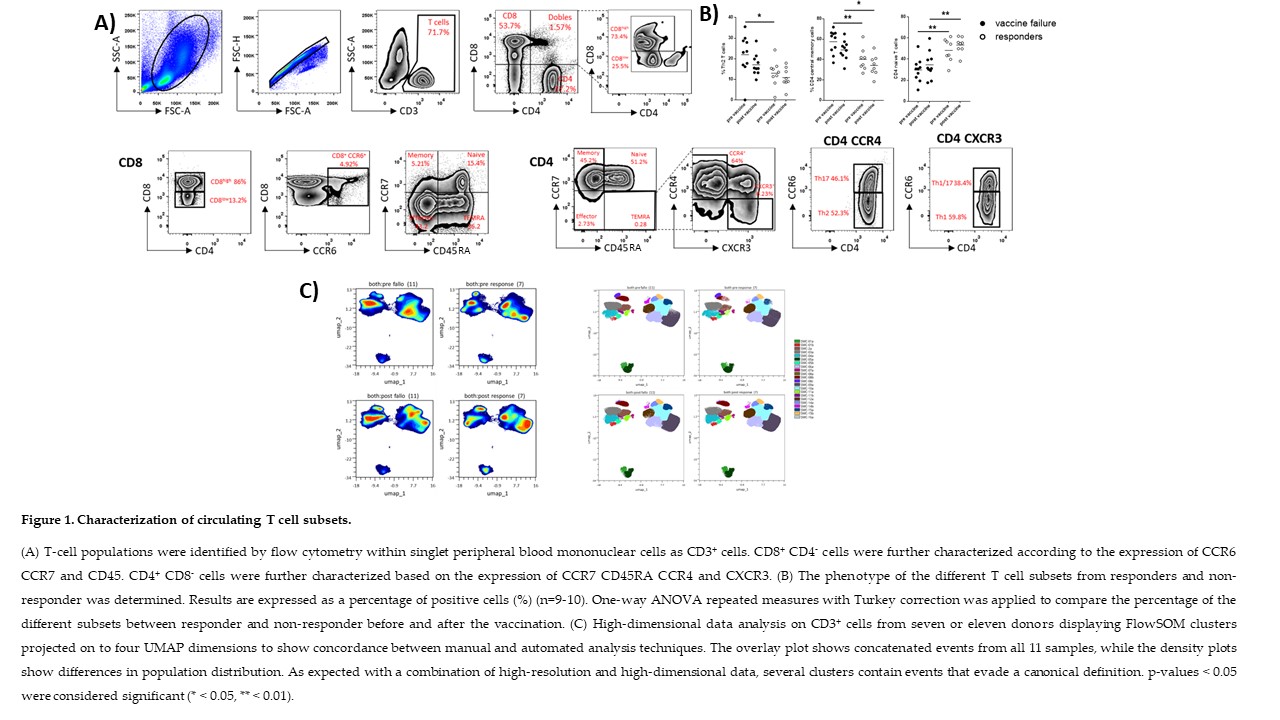
Non-responders displayed a lower percentage of naïve T cells compared with those who responded while responders had a lower percentage of Th2 and CD4 central memory subsets before vaccination. According to the high dimensional data analysis, 22 different T-cell metaclusters were identified (Fig. 1). Indeed, the percentage of type 2 conventional dendritic cells was increased following vaccination in both responders and non-responders, allowing us to identify 11 submetacluster (Fig. 2). Finally, The percentage of IgG class switch and IgG plasmablasts were increased following vaccination in the responders group, while the percentage of IgM plasmablast was increased in non-responders. Using the high dimensional data analysis 26 different subpopulations, were identified (Fig. 3).
Conclusion
The proportion of circulating T cell subsets can be used as predictor markers of the response to the HBV vaccine in IBD patients: while non-responders showed a lower percentage of naïve T cells, responders presented a lower percentage of Th2 T cells compared with their counterparts. The analysis of the data reveals that high-resolution and high-dimensional data, show several clusters containing events that evade the canonical definition.