P073 Eosinophil depletion partially protects from colonic inflammation, but increases colonic collagen deposition in a DSS colitis model
Jacobs, I.(1);Deleu, S.(2);Cremer, J.(1,2);Guedelha Sabino, J.(2,3);Ferrante, M.(2,3);Vermeire, S.(2,3);Breynaert, C.(1,4);Verstockt, B.(2,3);Vanuytsel, T.(2,3);
(1)KU Leuven, Microbiology- Immunology and transplantation, Leuven, Belgium;(2)KU Leuven, Chronic diseases and metabolism, Leuven, Belgium;(3)University Hostpitals Leuven, Gastroenterology and Hepatology, Leuven, Belgium;(4)University Hostpitals Leuven, General Internal Medicine, Leuven, Belgium;
Background
The role of eosinophils in intestinal inflammation and fibrosis in inflammatory bowel disease (IBD) is largely unknown. Therefore, we assessed the functional role of eosinophils in a chronic murine model of colitis and associated fibrosis via anti-CCR3 mediated eosinophil depletion.
Methods
6-8-week-old C57BL/6 RAG-/- mice received three cycles of dextran sodium sulphate (DSS) (1.75% - 2.25% - 2.25%) each interspersed with 14 days of recovery. Twice weekly, anti-CCR3 antibody (n=8), isotype (n=8) or saline injections (n=8) were given intraperitoneally. At the same timepoints, the disease activity index (DAI; mouse weight, stool consistency and presence of blood) was determined. At sacrifice, colonic damage was scored macroscopically (presence of hyperaemia, adhesions and length and degree of colon affected by inflammation). Colonic single cells were isolated and stained for flow cytometry, where eosinophils were characterized as CD45+ CD11b+ Siglec-F+ CD117- cells. Intestinal fibrosis was scored via colon weight/length, collagen deposition (using a colorimetric hydroxyproline assay) and COL1A1 expression by PCR.
Results
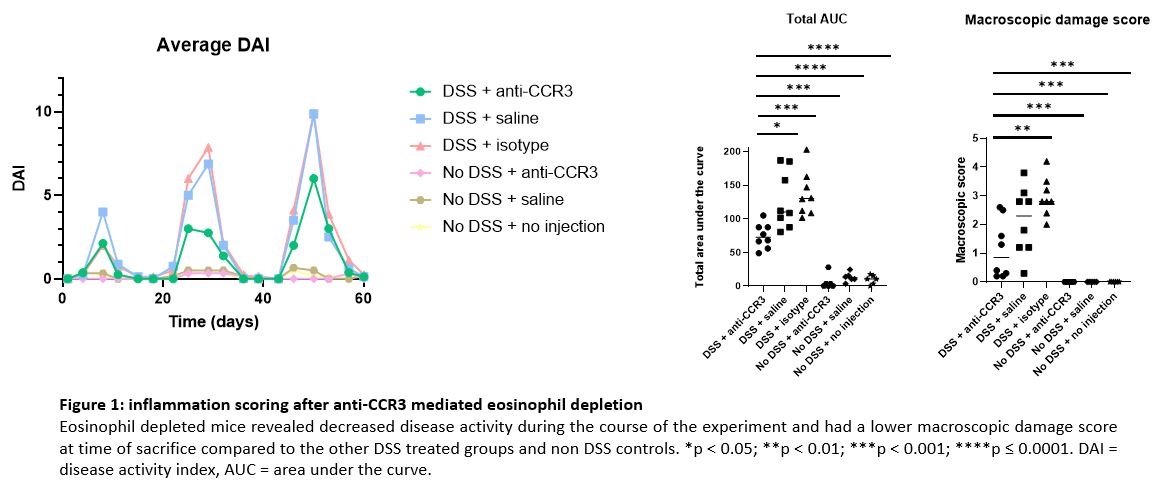
Anti-CCR3 mediated eosinophil depletion resulted in decreased disease activity compared to the other DSS treated groups injected with saline or isotype, determined by the area under the curve of the DAI (74.6±18.4 vs. 127.5±42.9 and 136.9±33.6, p=0.01 and p=0.0008 respectively) (figure 1). The macroscopic damage score also suggested eosinophil depleted mice to be partially protected from colonic inflammation compared to the saline and isotype injected mice that received DSS (1.1±1.0 vs. 2.1±1.2 and 3.0±0.7, p=0.09 and p=0.001 respectively) (figure 1). Colon weight/length and hydroxyproline assay showed a trend towards increased fibrosis in the anti-CCR3 injected group compared to saline (p=0.03 and 0.07, respectively) but not isotype (p=0.3 and 0.1, respectively) injected groups (figure 2). However, COL1A1 expression levels were significantly increased in the eosinophil depleted mice compared to the saline and isotype injected mice receiving DSS (43.2±11.4 vs. 23.3±8.7 and 30.1±11.0, p=0.002 and 0.04 respectively) (figure 2), indicating increased collagen deposition.
Conclusion
Eosinophil depletion via intraperitoneal anti-CCR3 injections resulted in partial protection against colonic inflammation, but was associated with increased collagen production. Caution is therefore needed when designing therapeutic interventions targeting eosinophils.