P111 Cross-sectional imaging is highly sensitive in detecting endoscopic post-operative recurrence in Crohn’s disease patients
Bachour, S.(1);Shah, R.S.(1);Lyu, R.(2);Nakamura, T.(3);Shen, M.(3);Li, T.(3);Rieder, F.(1);Cohen, B.(1);Qazi, T.(1);Lashner, B.(1);Achkar, J.P.(1);Philpott, J.(1);Lightner, A.(4);Holubar, S.(4);Regueiro, M.(1);Dane, B.(5);Baker, M.(6);Axelrad, J.(7);Click, B.(1);
(1)Cleveland Clinic Foundation, Department of Gastroenterology and Hepatology, Cleveland, United States;(2)Cleveland Clinic Foundation, Department of Quantitative Health Sciences, Cleveland, United States;(3)New York University Langone Hospital, Department of Internal Medicine, New York City, United States;(4)Cleveland Clinic Foundation, Department of Colorectal Surgery, Cleveland, United States;(5)New York University Langone Hospital, Department of Radiology, New York City, United States;(6)Cleveland Clinic Foundation, Imaging Institute, Cleveland, United States;(7)New York University Langone Hospital, Department of Gastroenterology, New York City, United States
Background
Postoperative Crohn’s disease (CD) surveillance relies on endoscopic monitoring. The role of cross-sectional imaging in post-operative CD surveillance is less clear. We aimed to evaluate radiographic characteristics, endoscopic concordance, and the predictive ability of imaging for postoperative recurrence (POR).
Methods
Multi-institution retrospective cohort study of adult CD patients who underwent ileocolonic resection (ICR) between 2009-2020. Patients with a CT or MR enterography within 90 days of a postoperative surveillance colonoscopy were included. Imaging studies were interpreted by blinded expert CD radiologists. Endoscopic activity was assessed by Rutgeerts’ scoring (POR ≥ i2b). Patients were categorized by presence of endoscopic POR (E+ or E-) or radiographic disease activity (R+ or R-) and grouped by endoscopic and radiographic concordance.
Results
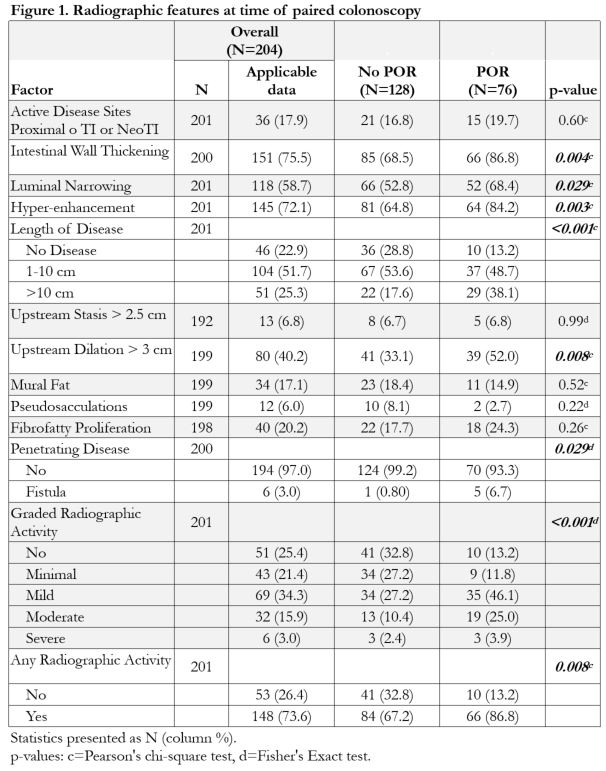
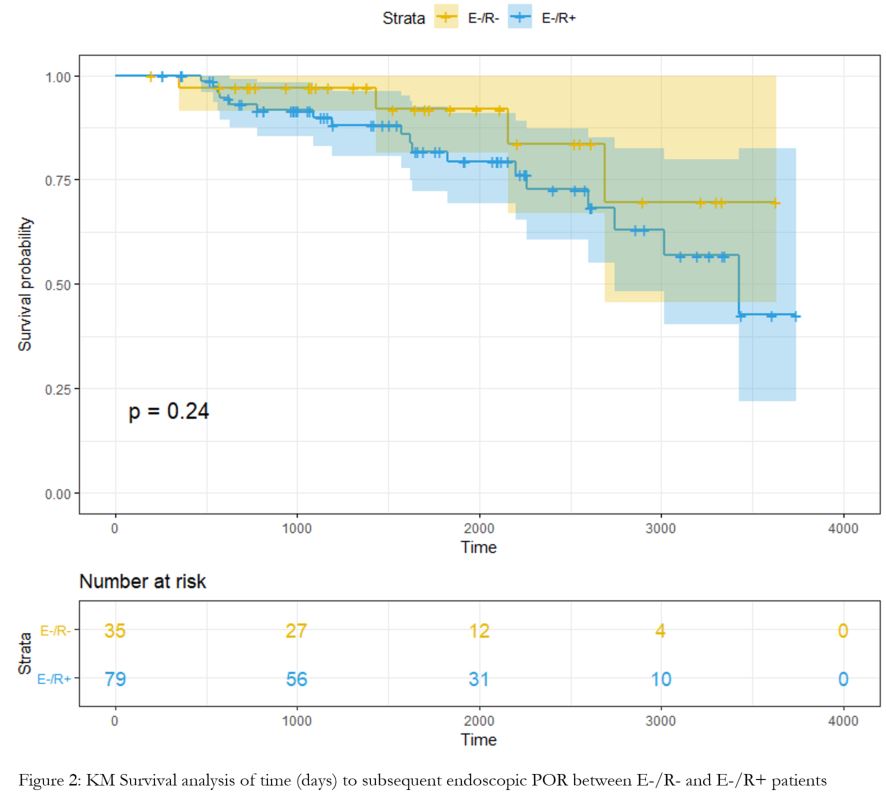
201 CD patients (57.7% female, mean age 31 years, 81.2% stricturing CD, 17.9% >1 prior ICR, 22.5%) with paired colonoscopy and imaging were included. Median time from ICR to paired endoscopy was 23.2 months. Imaging was highly sensitive for detecting POR (84.2%), but poorly specific (32.8%). The plurality (41.8%, N=84) were discordant E-/R+, 32.8% concordant positive (E+/R+), 20.4% concordant negative (E-/R-), and 5% discordant E+/R-. In patients with endoscopic POR, imaging detected intestinal wall thickening (86.8%; p=0.004) and hyper-enhancement (84.2%; p=0.003) at higher rates and corresponded with endoscopic severity (Figure 1). Multiple correspondence analysis showed association between severe endoscopic (i3/i4) disease and advanced radiographic disease. The majority (58.3 %) of E+/R- patients (N=12) had a Rutgeerts’ score of i2b. Majority of E-/R+ (N=84) had minimal/mild radiographic disease (81%). Differences in characteristics between the E-/R+ and E+/R+ was most pronounced in length of disease >10 cm (26.1%, 45.3%). Subsequent colonoscopies were performed in 74 E-/R+ (i0=28, i1=12, i2a=34) and 35 E-/R- (i0=20, i1=9, i2a=6) patients with 18 E-/R+ (24.3%; i0=8, i1=3, i2a=7) and 4 E-/R- (11.4%; i0=1, i1=2, i2a=1) patients developing POR (p=0.09). However, survival analysis between E-/R+ and E-/R- showed no difference to time to subsequent POR (p=0.24) (Figure 2). Imaging features at time of paired negative endoscopy did not predict subsequent endoscopic POR.
Conclusion
Cross-sectional imaging is highly sensitive to detect endoscopic POR; advanced radiographic disease correlates with increased endoscopic severity. Patients with no endoscopic recurrence in the presence of radiographic activity may require increased surveillance, though larger study cohorts are needed. Imaging compliments, but should not supplant, endoscopic POR surveillance paradigms.