P111 Gut barrier markers in Inflammatory Bowel Disease
Nguyen, A.(1);Sparrow, M.P.(2);Moore, G.(3);Gibson, P.R.(2);
(1)Monash University- Alfred Health and Monash Health, Gastroenterology, Melbourne, Australia;(2)Monash University and Alfred Health, Gastroenterology, Melbourne, Australia;(3)Monash University and Monash Health, Gastroenterology, Melbourne, Australia;
Background
Blood monitoring for disease activity in inflammatory bowel disease (IBD) is largely limited to C-reactive protein (CRP), but this may be raised in other inflammatory conditions and normal in active disease. Aims were to: (a) compare plasma levels of putative gut barrier markers, lipoprotein polysaccharide-binding protein (LBP), soluble CD14 (sCD14), syndecan-1 and intestinal fatty acid-binding protein 2 (IFABP2) in patients with IBD with those in controls; (b) define association with inflammatory activity; (c) examine responsiveness to change after biologic induction therapy.
Methods
Plasma was prospectively collected from patients with IBD and matched healthy controls. IBD was considered active with faecal calprotectin (FCP) ≥150 μg/g and/or an intestinal ultrasound showing a Limberg score ≥2. Gut barrier markers were compared to FCP and CRP. In a subset of patients who commenced on biologic therapy, they were measured at baseline and at least 14 weeks later. Biomarker concentrations were described as medians and spearman correlation was used for comparison with traditional biomarkers.
Results
101 patients with IBD and 51 controls were matched in age (33 vs 34 years) and gender (males 54% vs 47%). Treatment for IBD included aminosalicylates (38%), immunomodulators (47%), biologics (58%) and steroids (20%). In Crohn’s disease (n=60), distribution was ileal (45%), ileocolonic (30%) and colonic (25%); 31 had active disease. In ulcerative colitis (n=41), distribution was pancolitis (63%), left-sided (29%) and proctitis (7%); 18 had active disease. Compared with controls, patients with IBD had higher levels for LBP (13.6 vs 10.1 μg/ml; p<0.0001), sCD14 (1.3 vs 1.2 μg/ml; p<0.001) and LBP:sCD14 ratio (11 vs 8.8; p=0.002), but lower levels for syndecan-1 (19.4 vs 30 ng/ml; p=0.006) and IFABP2 (1452 vs 1696 pg/ml; p=0.015).
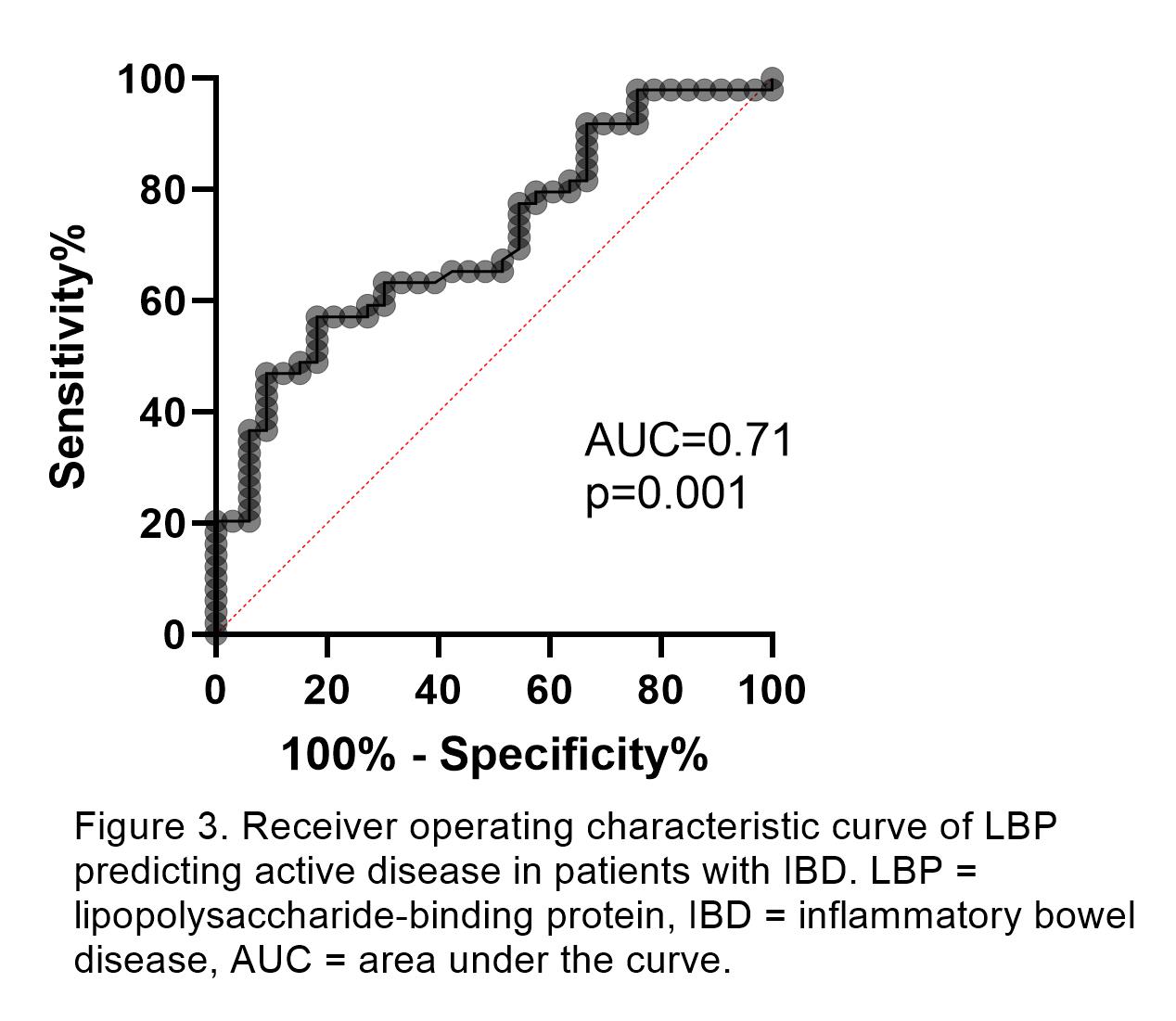
Only LBP differentiated between active and inactive disease in Crohn’s disease (16.1 vs 13.5 μg/ml; p=0.045) and ulcerative colitis (16.7 vs 10 μg/ml; p=0.012). LBP, and not other markers, correlated with FCP in all patients with IBD (r=0.46; p<0.001). LBP and sCD14 correlated with CRP (r=0.7 and r=0.46; p<0.001). The best cut-off value for LBP in detecting active disease was >15.9 μg/ml (AUC 0.71, sensitivity 57%, specificity 82%). In 18 patients who underwent biologic induction, LBP (17.1 to 13.8 μg/ml; p=0.094) and sCD14 (1.5 to 1.3 μg/ml; p=0.064) tended to fall.

Conclusion
Of putative barrier markers, only those associated with bacterial translocation (LBP, sCD14) were elevated in IBD with epithelial markers (syndecan-1, IFABP2) paradoxically reduced. Only LBP was associated with active disease though its responsiveness to therapy is uncertain and requires further prospective study.


