P112 S1PR expression on circulating immune cells is not limited to lymphocytes in patients with inflammatory bowel disease
Verstockt., B.(1,2)*;Verstockt, S.(2);Cremer, J.(3);Sabino, J.(1,2);Ferrante, M.(1,2);Vermeire, S.(1,2);
(1)University Hospitals Leuven, Dpt. Gastroenterology and Hepatology, Leuven, Belgium;(2)KU Leuven, Dpt. Chronic Diseases and Metabolism, Leuven, Belgium;(3)KU Leuven, Department of Microbiology- Immunology and Transplantation- Allergy and Clinical Immunology, Leuven, Belgium;
Background
With the recent approval of ozanimod in ulcerative colitis (UC) and promising data of etrasimod, S1P receptor (S1PR) modulators are entering the therapeutic landscape. Besides differences in receptor selectivity (ozanimod S1PR1/5, etrasimod S1PR1/4/5), both compounds induce a drop in circulating B/T-lymphocytes, without affecting monocyte counts. This lymphocyte drop seems independent of treatment response, suggesting that other cell types – like monocytes, implicated in IBD pathogenesis - might contribute to efficacy. Furthermore, very little is known about the expression of S1PR on circulating lymphocytes/monocytes in the context of IBD.
Methods
Peripheral blood mononuclear cells were isolated from 135 IBD patients with active endoscopic disease (Table 1), and subsequently FACS sorted (CD14 monocytes and CD4 T-cells). RNA was extracted from lysed cells, and single-end sequenced using Illumina HiSeq4000. 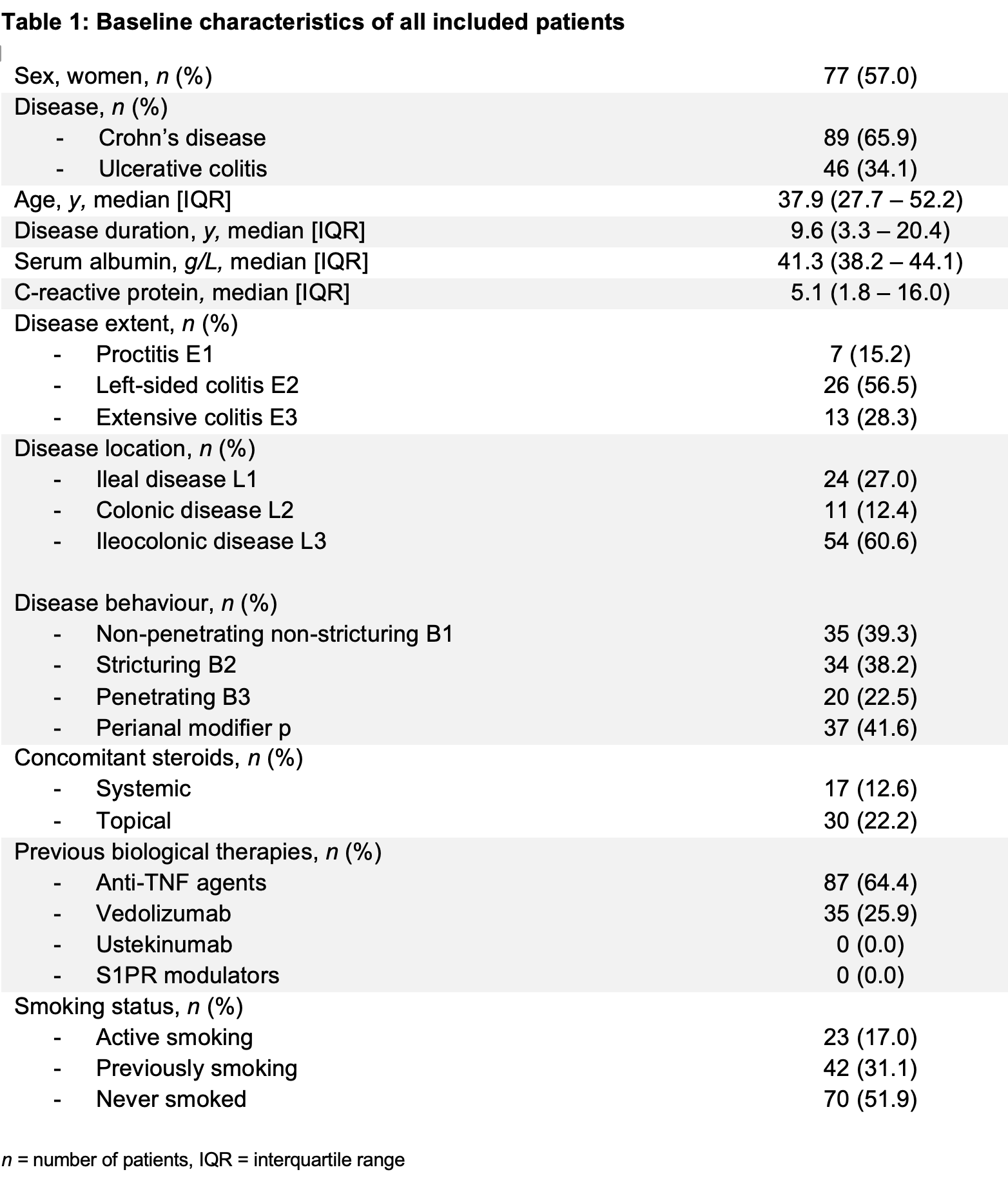
Results
All S1PR were identified on both CD4 T-cells and monocytes, though with hardly any S1PR5 expression on circulating monocytes and hardly any S1PR3 expression on T-cells. Receptor expression on both monocytes and T-cells correlated significantly only for S1PR1 (r0.25, p=0.003) and S1PR4 (r 0.19, p=0.02). Circulating T-cells had substantial higher expression of S1PR1 (fold change [FC] 1092.0, p<2.2E-16), S1PR2 (FC 1.84, p=5.3E-7), S1PR4 (p=2.4, p<2.2E-16) and S1PR5 (FC infinite, p<2.2E-16) compared to monocytes. In contrast, circulating monocytes expressed significantly more S1PR3 (FC infinite, p<2.2E-16). Receptor expression on T-cells did not differ between patients with Crohn’s disease (CD) and UC, whereas monocyte S1PR1 was significantly elevated in CD as compared to UC (FC 4.5, p=0.006) (Figure 1). Previous anti-TNF was not associated with any difference in S1PR1, but was associated with a slight increase in S1PR4 (FC=1.26, p=0.02). No association was observed in relation to previous vedolizumab exposure, whereas concomitant steroid use was linked to a decrease in S1PR5 on T-cells (FC 0.35, p=0.007). Disease duration or inflammatory burden (CRP) were not associated with any S1PR, though S1PR1 positively correlated with age in T-cells (r 0.23, p=0.008). In UC, S1PR1 on monocytes was significantly elevated in proctitis compared to left-sided and pancolitis (p=0.02); in CD, L1 disease was linked to elevated S1PR1 monocyte expression as compared to patients with L2/L3 (p=0.002). No link with CD disease behaviour could be demonstrated.

Conclusion
Besides lymphocytes, monocytes do express S1PR in patients with IBD. The clinical consequences and the potential link with efficacy of S1PR modulators should therefore be further explored, especially given the heterogeneity of S1PR expression on circulating cells in IBD patients.


