P114 SARS-CoV-2 infection in IBD: pandemic waves and predictors of severe or persistent COVID-19
Taxonera Samso, C.(1);Olivares, D.(1);Blanco , I.(2);Velasco, E.(2);Molina, S.(2);López , G.(2);López-García, O.N.(2);Alba, C.(1);Rey, E.(2);
(1)Hospital Clínico San Carlos, IBD Unit- Department of Gastroenterology, Madrid, Spain;(2)Hospital Clínico San Carlos, Gastroenterology, Madrid, Spain;
Background
This study aimed to compare the risk of COVID-19 in patients with IBD versus the general population, and to evaluate predictors of infection acquisition, progression to severe forms, and risk of developing persistent COVID-19. We also assess the differences between cases across the different COVID-19 pandemic waves in our target population.
Methods
This single-centre prospective, cohort study included consecutive IBD patients diagnosed of COVID-19 either by a positive polymerase chain reaction test and/or antigen test in nasopharyngeal swabs, or by anti-SARS-CoV-2 antibodies, and that they had a follow-up of at least 4 months. Using logistic regression, we evaluated cases versus IBD controls included in the IBD Unit database for predictors of COVID-19 acquisition. COVID-19 cases were distributed according to pandemic waves. Cox regression analysis was used for predictors of severe and persistent COVID-19.
Results
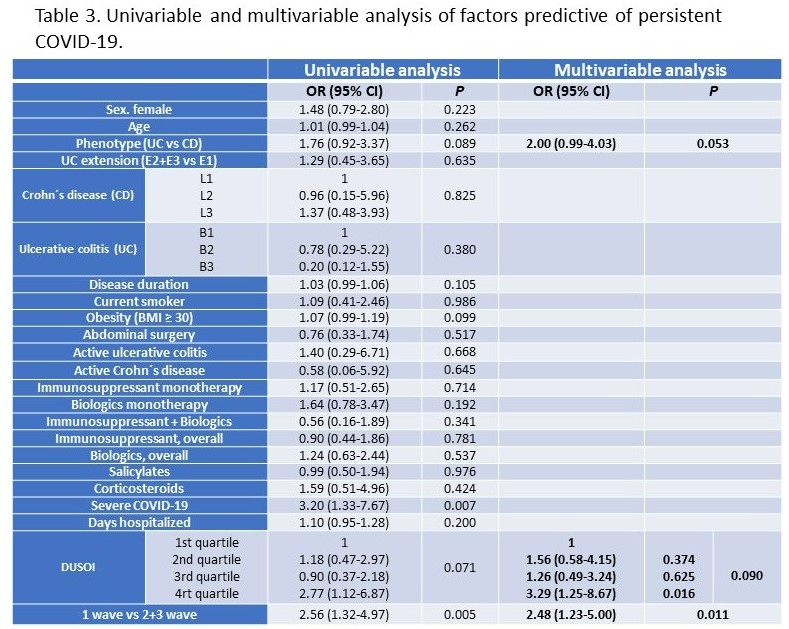
By May 31, 2021, 160 out of 1911 IBD patients (8.3%) were diagnosed with COVID-19. IBD patients had a similar adjusted incidence of COVID-19 (OR 0.94; 95% CI 0.86-1.02; P=0.42), and a similar associated mortality ratio (OR 0.83; 95% CI 0.6-1.06; P=0.48), compared to the general population. In multivariable analysis, treatment with biologics was associated with a higher risk (OR 2.22, P<0.001), and treatment with salicylates with a lower risk (OR 0.71, P=0.048) of contracting COVID-19.(Table 1) 62 COVID-19 cases were diagnosed during the first wave of pandemic (until the end of June 2020), and 54 and 44 cases during the second and third waves (until the end of December 2020 and May 2021, respectively).(Figure 1) In multivariate analysis, first wave cases were associated with a higher risk of progression to severe forms of infection (OR 4.76, 95% CI 1.83-12.37, P=0.001), and development of persistent COVID-19 (OR 2.4, 95% CI 1.16-4.95, P=0.018). 29 patients (18.1%) required hospitalisation and were classified as severe COVID-19, which was associated in multivariable analysis with age>48 (HR 3.68, P=0.007), cases diagnosed in the first wave (HR 6.04, P<0.001), and comorbidities (evaluated with Duke Severity of Illness Checklist [DUSOI], P<0.001).(Table 2) During a median follow-up of 8.4 months, 68 patients (42.5%) were diagnosed with persistent COVID-19. Multivariable analysis identified UC (P=0.053), comorbidities (P=0.090), and being diagnosed during the first wave (P=0.011) as risk factors for persistent COVID-19.(Table 3)


Conclusion
IBD patients have a similar risk of COVID-19 and associated mortality as the general population. Cases diagnosed during the first wave of the pandemic had severe and persistent forms of COVID-19 more frequently. Age and comorbidity were the main risk factors for severe forms of the disease.


