P117 Patient perceptions about causes of flare in IBD: results from the baseline dataset of the PREdiCCt study
Siakavellas, S.(1);Derikx, L.(1,2);Derr, L.(1);Williams, L.(1);Plevris, N.(1);Jenkinson, P.(1);Laura, L.(1);Constantine-Cooke, N.(3);Covil, K.(1);Murdoch, L.(1);Jones, G.R.(1,4);Lees, C.(1,5);
(1)Western General Hospital- NHS Lothian, Edinburgh IBD Unit, Edinburgh, United Kingdom;(2)Radboud University Medical Center- Nijmegen- the Netherlands, Inflammatory Bowel Disease Center- Department of Gastroenterology and Hepatology, Nijmegen, The Netherlands;(3)Institute of Genetics and Molecular Medicine- University of Edinburgh, MRC Human Genetics Unit, Edinburgh, United Kingdom;(4)The Queen's Medical Research Institute- University of Edinburgh-, Centre for Inflammation Research, Edinburgh, United Kingdom;(5)Institute of Genetics and Molecular Medicine- University of Edinburgh, Centre for Genomics and Experimental Medicine, Edinburgh, United Kingdom PREdiCCt Study Writing Group
Background
Patient reported outcomes are important endpoints in IBD management, but patient perceptions of the causes of disease flare are unknown and thus may reveal novel areas for future study.
Methods
The PREdiCCt study (https://www.predicct.co.uk) is the largest prospective study of the causes of IBD flare. 2629 patients in clinical remission were recruited from 48 UK sites and followed for 2 years with detailed assessment of environmental and dietary factors via monthly questionnaires. 1946 (74%) patients completed the baseline questionnaires. We present here the results of the baseline questionnaire analysis of patient perceptions of disease flare, derived from a list of 17 putative causes from the literature and their own experience via free text input.
Results
In total 1,946 IBD patients [male=852, CD=1000; UC/IBDU=946, age 45.8±15.5 (mean±SD in years)] gave their opinion about factors initiating a flare. The commonest causes reported were stress (n=1359, 69.8%), dietary changes (n=911, 46.8%), alcohol use (n=385, 19.8%), sleep disturbances (n=331, 17%) and that their medication stopped working (n=308, 15.8%) (Figure 1). CD participants were more likely to identify dietary changes (50% vs 43%, p<0.001) and menstruation (16% vs 10% of female patients, p<0.001) as flare triggers than UC/IBDU participants, while UC/IBDU participants more frequently reported loss of response to medication as a trigger for flare (9% vs 5% for CD participants, p<0.001). CD patients with small bowel involvement were more likely to name dietary changes (61% vs 42%, p<0.001), travel (14% vs 9%, p=0.016) and smoking (4% vs 1%, p=0.04) as flare triggers. When compared by gender, the ranking of causes was identical but female participants were more likely to identify stress (77% vs 65%, p<0.001) and antibiotic use (12% vs 6%, p<0.001) as reasons for disease relapse compared to male participants.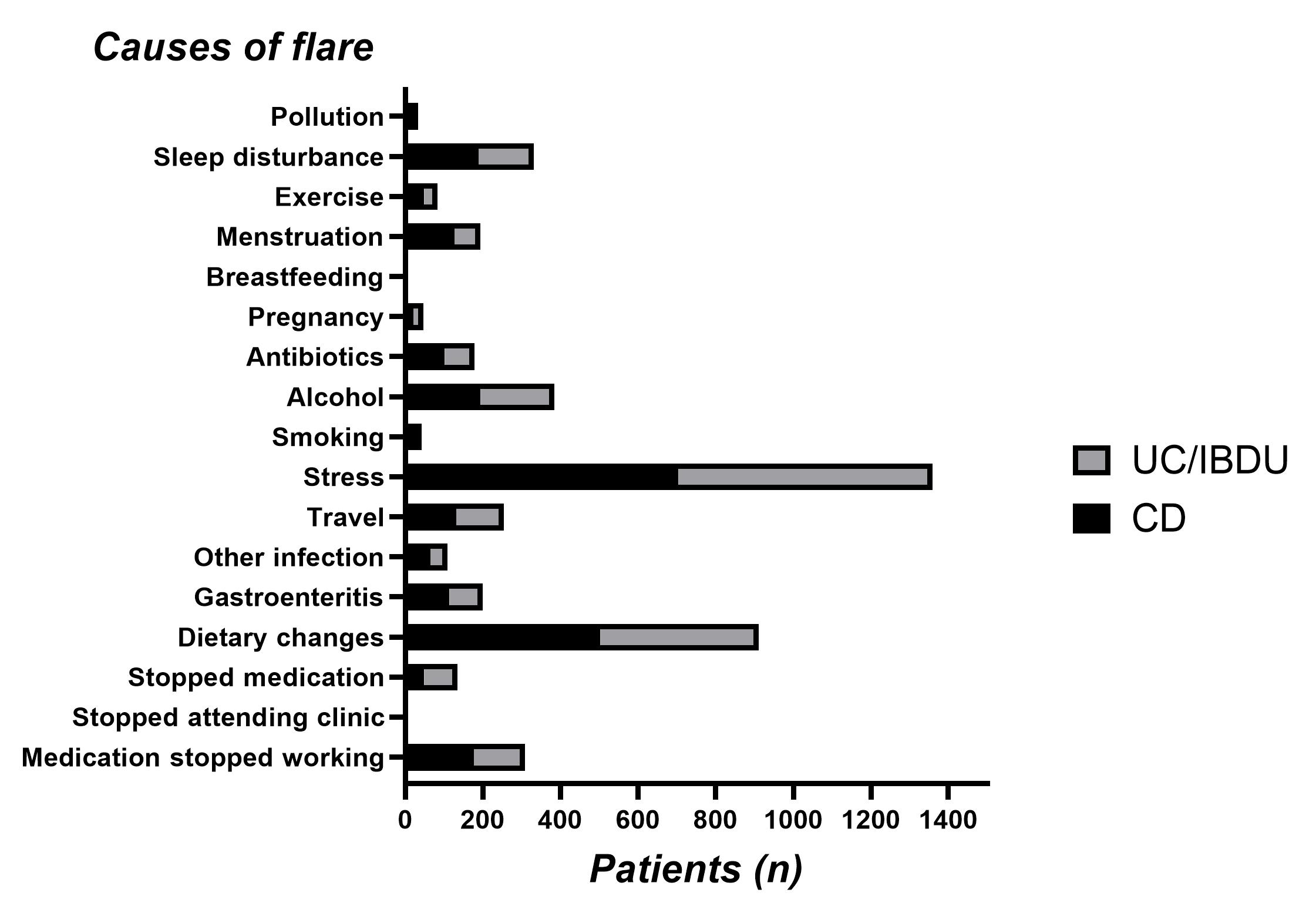
Conclusion
Stress, dietary changes and alcohol use were identified as the main causes of flare by patients with dietary changes more frequently reported in CD (especially those with small bowel involvement). The impact of environmental and dietary factors in the development of flare is being further investigated with ongoing longitudinal data collection in the PREdiCCt Study.


