P126 Ask twice: The importance of repeated faecal calprotectin testing prior diagnostic colonoscopy in an adult inception cohort.
Rimmer, P.(1)*;Cheesbrough, J.(1);Quraishi, M.N.(1);Sharma, N.(1);Cooney, R.(1);Love, M.(1);Iqbal, T.(1);
(1)University Hospitals Birmingham NHS Foundation Trust, Gastroenterology, Birmingham, United Kingdom;
Background
Elevated Faecal Calprotectin (FCP) is established as a valuable tool in differentiating Inflammatory Bowel Disease (IBD) from Irritable bowel syndrome (IBS) and monitoring IBD activity. Initial implementation studies in the UK demonstrated benefit from repeat testing to exclude false positives. This is not currently mandated by IBD consensus guidelines. Growing waiting times are increasing pressure to include a single result in straight to test pathways. No one level for significant elevation is defined with levels between 100-250ug/g used. We present our experience of the real-world utility of FCP used in a primary care referral pathway.
Methods
From Jan 2021-Nov 2022, new referrals were streamed into a rapid access ‘Inception IBD’ clinic on the basis of symptoms and raised FCP. A repeat FCP (kit sent in advance) was brought to the first appointment, with same day processing using the Buhlmann fCAL Turbo Test. Results and accompanying diagnosis and outcome data was collected prospectively. There was no standardised testing interval but median time from referral to review was 34 days.
Results
A single FCP was available for 425 patients with a final diagnosis. Two pre-treatment FCPs were available in 185. Median initial FCP was 949ug/g in those subsequently diagnosed with IBD (Ulcerative colitis 1162ug/g, Crohn’s 893ug/g) vs 353ug/g in those without IBD. This difference heightened on retesting, with median FCP in IBD 749ug/g vs 34ug/g in non-IBD (Fig 1). FCP fell between 1st and 2nd measurement in 88.6% of patients who had IBD excluded.
In IBD, baseline FCP showed strong correlation with established disease activity markers (Fig 2).

Baseline FCP levels were significantly higher in IBD patients who went on to require biologic treatment (Mann-Whitney U 2763, p<0.001).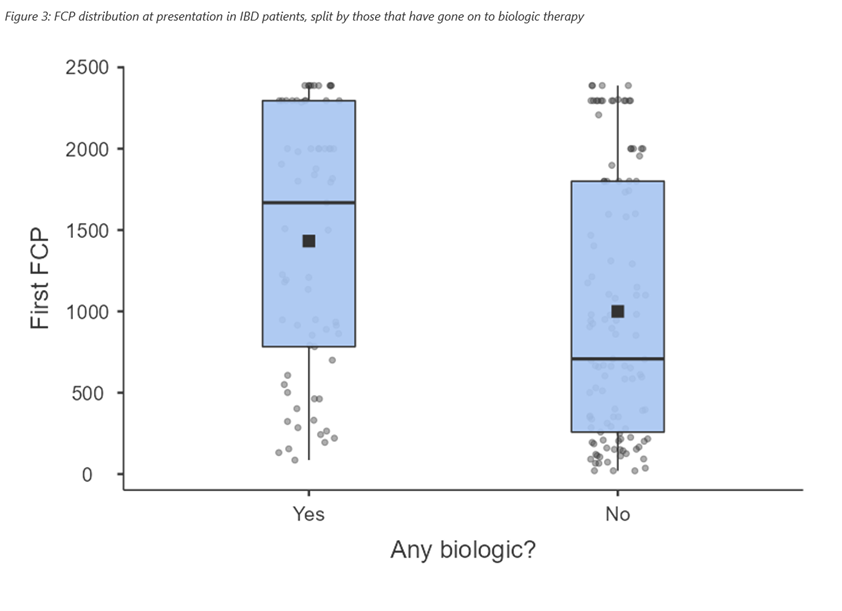
A variety of FCP cut-off values were assessed (Fig 4). A two sample >200ug/g cut off performed best as assessed by Area Under the Curve (AUC). However, sensitivity fell to 81.5% at this level.
Of 15 IBD patients who didn’t have two FCPs >200ug/g, 7 had an increase between the 1st and 2nd FCP (median 147 vs 487ug/g). The remaining 8 comprised 4 ileal Crohn’s, 3 mild proctitis and 1 stricturing colonic Crohn’s in whom FCP failed to correlate with disease activity. Overall, 83% (48/58) of patients with increasing 1st to 2nd FCP were diagnosed with IBD.
Conclusion
Our data supports repeat testing of FCP to avoid unnecessary investigations adding to post COVID endoscopy backlogs. A cut off of two values >200ug/g had the best overall performance but can miss a small number of IBD cases, particularly those with isolated ileal disease or a more indolent disease course. This cut off should not be used in those with a marked increase between 1st and 2nd result, where IBD is likely.


