P141 Risk Factors of Atherosclerotic Cardiovascular Disease (Ischemic Heart Disease and Cerebrovascular Accident) in Patients With Inflammatory Bowel Disease: a hospital-based cohort
Muiño, D.(1);Carballo-Folgoso, L.(1)*;Ortega-Carriedo , J.(2);Flórez-Díez, P.(1);de Francisco, R.(1,3);Pérez-Martínez, I.(1,3);Castaño-García, A.(1);Fernández-González, E.(1);García-Pérez, C.(3);Martínez-González, S.(3);Rolle, V.(3);Riestra, S.(1,3);
(1)Hospital Universitario Central de Asturias, Gastroenterology, Oviedo, Spain;(2)Universidad de Oviedo, Medicine, Oviedo, Spain;(3)Instituto de Investigación Sanitaria del Principado de Asturias ISPA, Diet Microbiota and Health, Oviedo, Spain;
Background
Immune-mediated inflammatory diseases (IMIDs) involve an increased risk of developing atherosclerotic cardiovascular disease (ASCVD). However, the association between inflammatory bowel disease (IBD) and ASCVD is not well established. Our aims were to evaluate the frequency of ASCVD [ischemic heart disease (IHD) and cerebrovascular accident (CVA)] after IBD diagnosis and to identify the risk factors associated with its development.
Methods
Observational, single-centre study which included all patients seen at the IBD Unit of the Hospital Universitario Central de Asturias (Spain) between May 2010 and April 2022. Cardiovascular risk factors and the development of ASCVD were prospectively assessed; in addition, this information was sought selectively prior to IBD diagnosis and patients’ first visit to the unit. Regarding classical risk factors, we analysed hypertension, dyslipidaemia and diabetes mellitus. As possible risk factors related to IBD, we analysed the presence of complex IBD which, in the case of Crohn's disease (CD), we defined as the presence of stricturing or penetrating behaviour or the need for bowel resection surgery, and, in the case of ulcerative colitis (UC), as an E3 extension or the need for colectomy. Finally, we analysed the coexistence of other IMIDs as a risk factor.
Results
A total of 2,153 patients were included (52% CD, 45% UC and 3% IBD-unclassified). Forty-nine percent were women and mean age at IBD diagnosis was 39 years. Twenty-four percent had hypertension, 14% dyslipidaemia and 8.6% diabetes; 59% were current or former smokers; 37% had an associated IMID (12% cutaneous and 7.9% joint). Prior to IBD diagnosis, 62 patients had presented with ASCVD (41 IHD and 21 CVA). After IBD diagnosis, 95 patients had at least one ASCVD (49 IHD and 46 CVA); after 31,516 patient-years of follow-up, the incidence of a first ASCVD was 0.31 per 100 patient-years (0.16 IHD and 0.15 CVA). The incidence of ASCVD was stable over time after IBD diagnosis. In the multivariate analysis (Table 1), age at IBD diagnosis >50 years (p<0.001), hypertension (p=0.006), dyslipidaemia (p=0.032), male sex (p=0.004) and a history of ASCVD prior to IBD diagnosis (p=0.011) were associated with an increased risk of ASCVD. With these variables, a Cox regression survival analysis was performed (Figure 1 and 2). Neither the type of IBD, the existence of complex IBD nor the coexistence of other IMIDs was associated with an increased risk of ASCVD.
Table 1.
Figure 1.
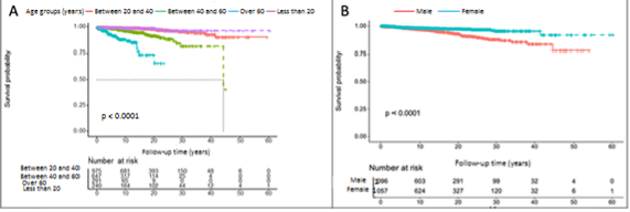
Figure 2.

Conclusion
The development of ASCVD in patients with IBD is associated with classical risk factors (hypertension and dyslipidaemia), as well as older age at diagnosis and male sex. The coexistence of other IMIDs does not increase the risk of ASCVD in these patients.


