P178 Evaluation of the Ulcerative Colitis Intestinal Ultrasound (UC-IUS) Index in Pediatric patients with newly diagnosed ulcerative colitis
Hudson, A.(1);Ma, H.(1);Lo, C.(1);Kim, J.(1);Kuc, A.(1);Novak, K.(2);Carroll, M.(1);Wine, E.(1);Isaac, D.(1);HuynhDr, H.(1)*;
(1)University of Alberta, Department of Paediatrics- Division of Gastroenterology and Nutrition, Edmonton, Canada;(2)University of Calgary, Department of Medicine- Division of Gastroenterology and Hepatology, Calgary, Canada;
Background
Transabdominal bowel ultrasound (TABUS) is a non-invasive tool that can be used to assess bowel inflammation in ulcerative colitis (UC). It is particularly attractive for use in children, given the need for general anesthesia when undergoing endoscopic assessment of bowel inflammation. A standardized TABUS scoring system in UC has only been developed in adults (the UC Intestinal Ultrasound (UC-IUS) Index). Our aim was to evaluate the UC-IUS Index in Pediatric patients.
Methods
Pediatric patients (<18 years old) with suspected UC were prospectively enrolled. TABUS was performed for the right side colon, transverse, descending, and sigmoid colons. UC-IUS Index scores were calculated: bowel wall thickness (BWT) (>2mm=1, >3mm=2, >4mm=3), Doppler signal (spots=1, stretches=2), haustrations (abnormal=1), and fat wrapping (present=1). Mayo endoscopic subscore (for each segment), Pediatric Ulcerative Colitis Activity Index (PUCAI), and inflammatory biomarkers were collected. Non-parametric tests were used to correlate UC-IUS and BWT with Mayo endoscopic subscores. Receiver operating characteristic (ROC) analyses evaluated the UC-IUS Index BWT cut-offs.
Results
Fifty-two patients (56% male) were included (Table 1). Data for 206 colonic segments were analyzed (2 segments missing due to 1 incomplete colonoscopy). Total UC-IUS scores significantly correlated with CRP (rho=0.61), albumin (rho=-0.49), PUCAI (rho=0.54), FCP (rho=0.41). UC-IUS Index scores and mean BWT for each segment showed significant moderate correlations with Mayo sub-scores of that segment (rho=0.60 and rho=0.58, respectively) (p<0.001) (Fig 1). These correlations were strong in the right colon (rho=0.77, rho=0.69), and moderate in the transverse (rho=0.52, rho=0.56), descending (rho=0.43, rho=0.50), and sigmoid (rho=0.50, rho=0.46) colons (p<0.01). The adult UC-IUS 2mm cut-off (Mayo 0 vs. Mayo 1-3) performed similarly in our Pediatric patients (sensitivity 80%, specificity 96%, area under the curve (AUC) 0.92). The 3mm (Mayo 0-1 vs. Mayo 2-3) and 4mm (Mayo 0-2 vs. Mayo 3) cut-offs had lower sensitivity (sensitivity 44%, specificity 98%, AUC 0.87; sensitivity 59%, specificity 92%, AUC 0.80) (Fig 2). Thinner BWT cut-offs performed better: 2.5mm (sensitivity 65%; specificity 89%) and 3.5mm (sensitivity 71%; specificity 86%).

Fig 1:
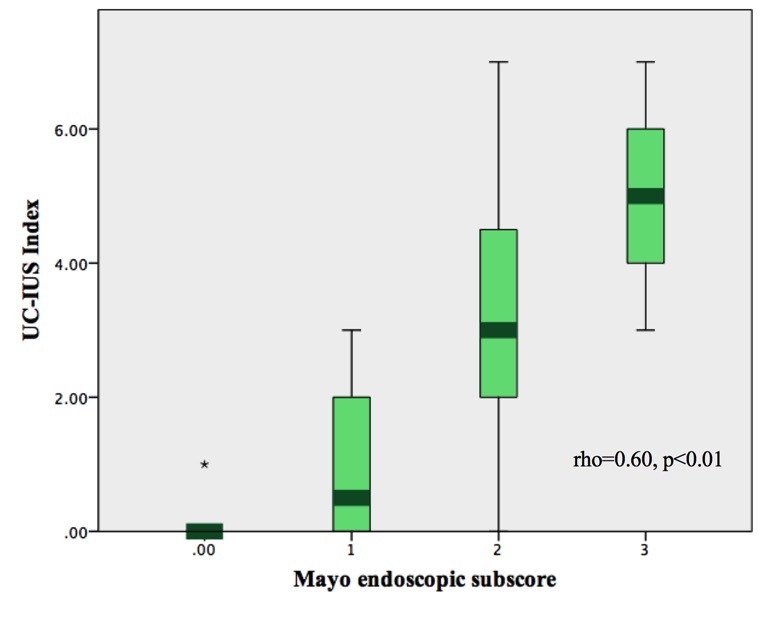
Fig 2:

Conclusion
In Pediatric patients with newly diagnosed UC, TABUS was a useful tool, with the UC-IUS and BWT correlating well with their endoscopic, clinical, and biochemical disease activity. Compared to the adult UC-IUS Index, Pediatric patients need a thinner BWT cut-off to better discriminate between mild vs. moderate/severe disease (2.5mm instead of 3mm) and mild/moderate vs. severe disease (3.5mm instead of 4mm).


