P188 Role of gastrointestinal ultrasound in severe Ulcerative Colitis: a real-life observational study from a tertiary center in Spain.
Rueda Sanchez, J.(1);Suarez Ferrer, C.J.(2);Poza Cordon, J.(2);Camara Baena, S.(3);Keco Huerga, A.(1);Garcia de la Borbolla Serres, J.(1);Martin Arranz, E.(2);Sanchez Azofra, M.(2);Rueda Garcia, J.L.(2);Garcia Ramirez, L.(2);Noci Belda, J.(2);Verges Martinez-Meco, T.(2);Martin Arranz, M.D.(2);
(1)Hospital Universitario Virgen de Valme, UGC Aparato Digestivo, Sevilla, Spain;(2)Hospital La Paz Institute for Health Research - IdiPAZ La Paz University Hospital - Universidad Autonoma de Madrid, IBD Unit, Madrid, Spain;(3)San Juan de Dios del Aljarafe Hospital, CMU Gastroenterology, Bormujos, Spain;
Background
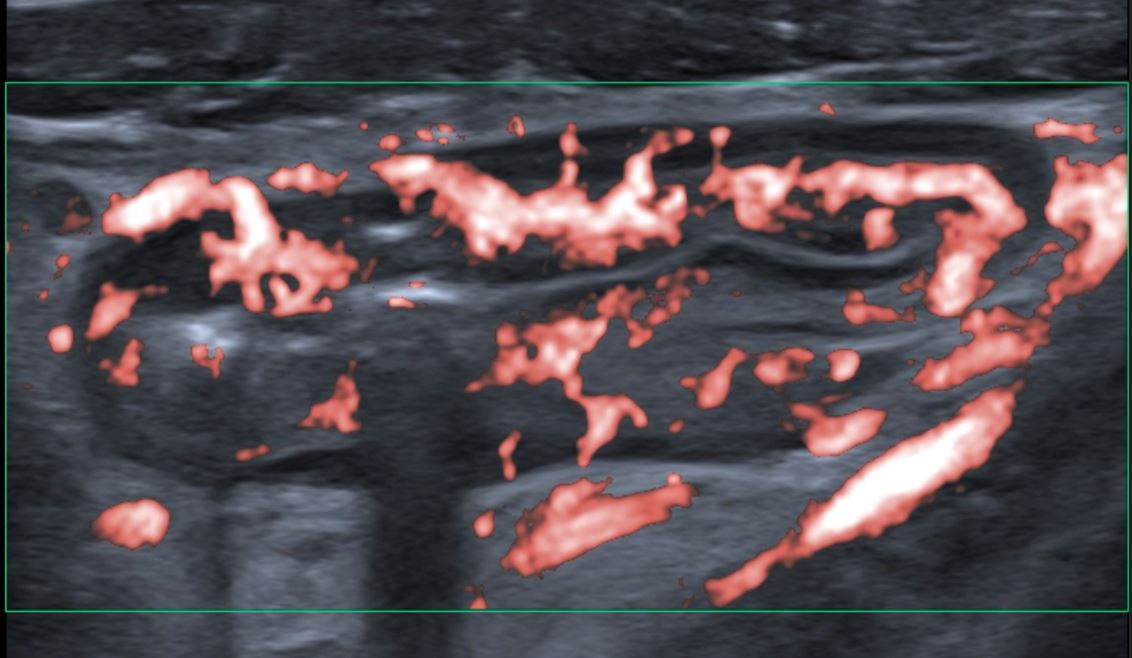
Gastrointestinal ultrasound (GIUS), applied to Crohn`s Disease, has proven correlation with imaging studies and endoscopy in terms of diagnosis, follow-up and evaluation of transmural complications. However, real-world data about Ulcerative Colitis (UC) patients is still scarce. The aim of our study was to evaluate GIUS role in severe UC patients from our real-life cohort.
Methods
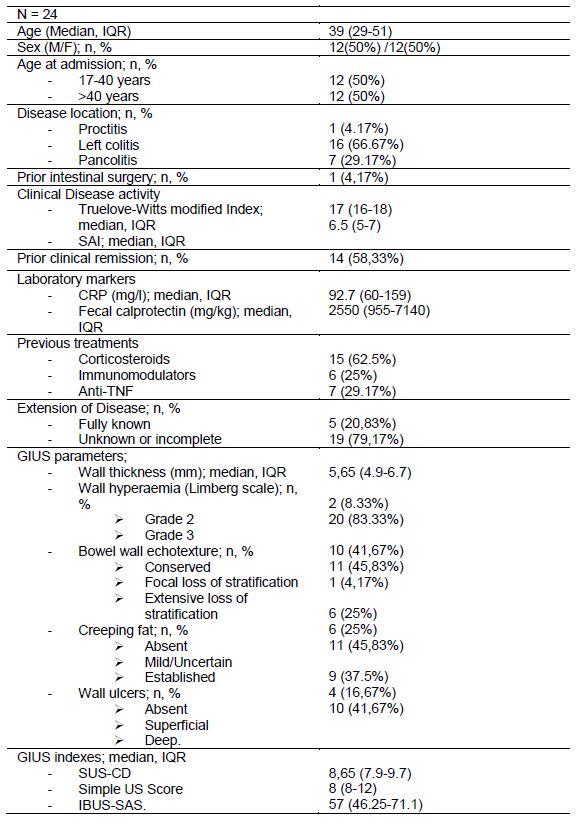
We present a retrospective observational study from a single tertiary center. We included adult UC patients who needed hospital admission due to severe disease activity, defined as Truelove-Witts Index (TW) 15 or higher and Simple Activity Index (SAI) 4 or higher. We assessed clinical (TW, SAI) and biomarker (CRP, calprotectin) evolution along hospitalization, need for biological treatment, steroid (CS) therapy or surgery, apart from GIUS parameters (wall thickness, wall hyperaemia, wall echotexture, creeping fat, wall ulcers), GIUS indexes (SUS-CD, Simple US Score, IBUS-SAS) and endoscopic findings (UCEIS) coming from a baseline exam. Statistic analysis was performed using Pearson’s Correlation coeficient, multivariant análisis, and Spearman`s Correlation coeficient between GIUS indexes.
Results
We included 24 patients, with a mean extensión of 66.67% left colitis and a 29.17% pancolitis. Severity of disease at admission is described as a mean SAI 6.16 and a mean TW 17.25, with a mean fecal calprotectin of 3643. A 29% of patients were treated previously with biological therapy.
Referring to GIUS parameters, median wall thickness was 5.65mm, with a 83.33% of patients presenting a Limberg grade 3 of wall hyperaemia. Wall ulcers were present in a 58.34% of patients, and established creeping fat was present in a 45.83% of patients. Mean score of GIUS indexes was SUS-CD 8.65, Simple US Score 8, and IBUS-SAS 57.
GIUS proves to be an useful tool to assess diagnosis and delimit extension of disease. A 79% of patients presented unknown extension of disease at the time of admission, mostly due to incomplete colonoscopy at diagnosis. GIUS describes full extension of disease in all the patients of the study.
In statistic análisis, our main finding is that Simple US Score proved statistic relationship with CS response during admission (Patients who responded to CS presented a mean Simple US Score 2.5 points lower than non-responders, p = 0.03). No isolated GIUS parameter proved relationship with CS response during admission. .jpg)
Conclusion
According to our results, GIUS is an effective tool for assessing diagnosis and extensión of disease in severe UC. Also, Simple US Score seems to be a reliable predictor of CS response during admission. Larger studies are needed to determine GIUS usefulness for predicting natural history of CU and need for CS or biological therapy.