P197 A biomarker of early mucosal destruction: Neutrophil-mediated type IV collagen degradation is elevated in patients with Crohn’s Disease and Ulcerative Colitis
Sorokina Alexdóttir, M.(1)*;Pehrsson, M.(1);Karsdal, M.A.(1);Godskesen, L.E.(2);Krag , A.(3);Kjeldsen , J.(2);Mortensen, J.H.(1);
(1)Nordic Bioscience, Biomarkers and Research, Herlev, Denmark;(2)Odense University Hospital, Department of Medical Gastroenterology, Odense, Denmark;(3)Odense University Hospital, Department of Gastroenterology and Hepatology, Odense, Denmark;
Background
Inflammatory bowel disease (IBD) is characterized by chronic inflammation due to an uncontrolled immune response orchestrated through, i.e. neutrophils. The basement membrane acts as a front-line defense promoting tissue integrity, where the α-3 chain of type IV collagen is solely expressed on the outermost layer of the mucosa. Detection of subclinical ulceration is crucial since early-stage IBD presents a unique window of opportunity for intervention, as the disease might become a self-sustaining process once deep inflammation becomes established. We therefore, wanted to develop a biomarker reflecting early tissue injury, aiding in the implementation of prompt treatment.
Methods
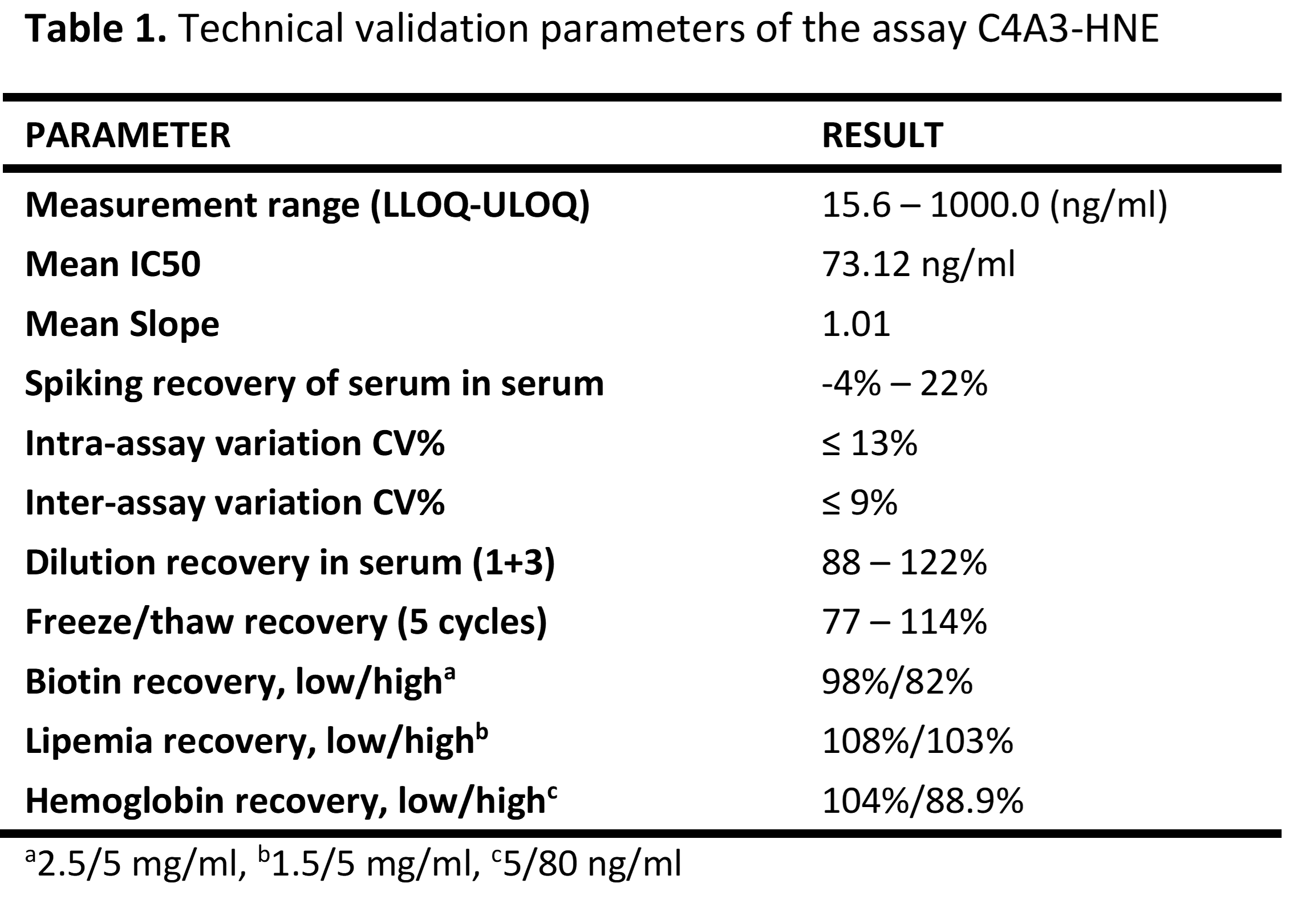
A competitive enzyme-linked immunosorbent assay quantifying a human neutrophil elastase (HNE) degraded fragment of type IV collagen α-3 chain was developed (C4A3-HNE). Dilution- and spiking recovery, inter- and intra-variability, and interference were evaluated. Acceptance criteria for technical validation were a recovery of 100% ±25 and an inter-intra variability of <15%. Commercial serum samples were purchased from ProteoGenex. Biological relevance was validated in an observational study from Odense University Hospital (OUH) and healthy controls. Groups were compared using Kruskal Wallis (Dunn‘s corrected).
Results
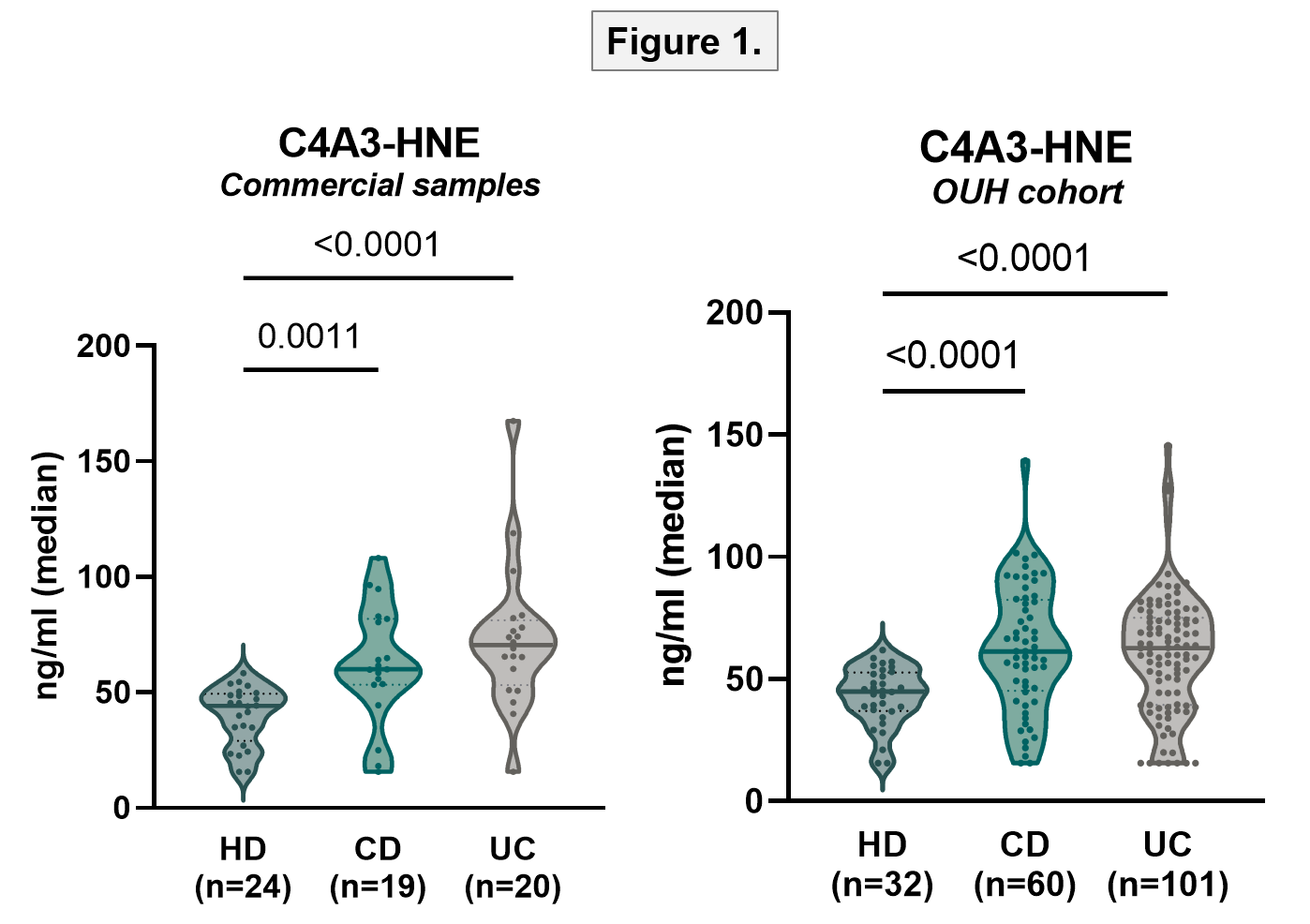
The technical validation of the C4A3-HNE assay demonstrated acceptable results for recovery, variation, and interference (table 1). Biological relevance was assessed in commercial IBD samples and healthy donors. C4A3-HNE was elevated in both CD and UC compared to healthy (p=0.001 and <0.0001)(AUC [95% CI]: 0.820 [0.669-0.971]; 0.875 [0.775-1.000]). The results were validated in a cohort of IBD patients (both p<0.0001)(fig.1). For UC, analysis showed that compared to patients in endoscopic remission, C4A3-HNE is elevated in patients with mild endoscopic activity, decreasing dose-dependently for moderate and severe disease. Fecal calprotectin and CRP levels were also lower in IBD patients with high levels of C4A3-HNE (fig.2). With a cut-off value of 54.1 ng/ml, C4A3-HNE could significantly discriminate between mild and severe endoscopic disease (table 2).


Conclusion
Our study demonstrates the biological and possible clinical relevance of the novel C4A3-HNE biomarker. The biomarker is elevated in patients with IBD compared with healthy, and high levels may reflect early mucosal damage in patients with UC. Furthermore, inflammatory markers were lower in IBD patients with high levels of C4A3-HNE, pointing towards high levels being indicative of early disease. C4A3-HNE may provide early detection of mucosal damage; however, further studies are required to assess the clinical validity of this biomarker.


