P200 The diagnostic yield of pan-enteric capsule endoscopy in inflammatory bowel disease: A systematic review and meta-analysis
Tamilarasan , A.G.(1);Tran , Y.(2);Paramsothy , S.(1);Leong , R.(1);
(1)Concord Repatriation General Hospital, Gastroenterology and Hepatology, Concord, Australia;(2)Macquarie University, Faculty of Medicine and Health Sciences, Sydney, Australia;
Background
Capsule endoscopy (CE) is a non-invasive diagnostic modality enabling real time video imaging of the gastrointestinal (GI) mucosa with an ingestible recording device. Major technological advancements now allow pan-enteric capsule endoscopy (PCE) to thoroughly assess the entire GI tract. CE is increasingly utilised in the inflammatory bowel disease (IBD) diagnostic algorithm. Our aim was to evaluate the diagnostic accuracy of PCEs in IBD.
Methods
We comprehensively searched electronic databases (MEDLINE, SCOPUS, EMBASE and Cochrane Central Register of Controlled Trials) for studies comparing the diagnostic accuracy of PCE with colonoscopy or magnetic resonance enterography (MRE). Prospective studies with ≥ 10 IBD patients were included in our final analysis. Diagnostic accuracy and yield were calculated for the detection of active IBD. Meta-analysis of proportions was performed to assess for an incremental benefit between modalities. The risk of bias was determined by the Quality Assessment of Diagnostic Accuracy in Systematic Reviews (QUADAS-2). Data was analysed by calculating forest plots and the use of the I2 statistic for heterogeneity.
Results
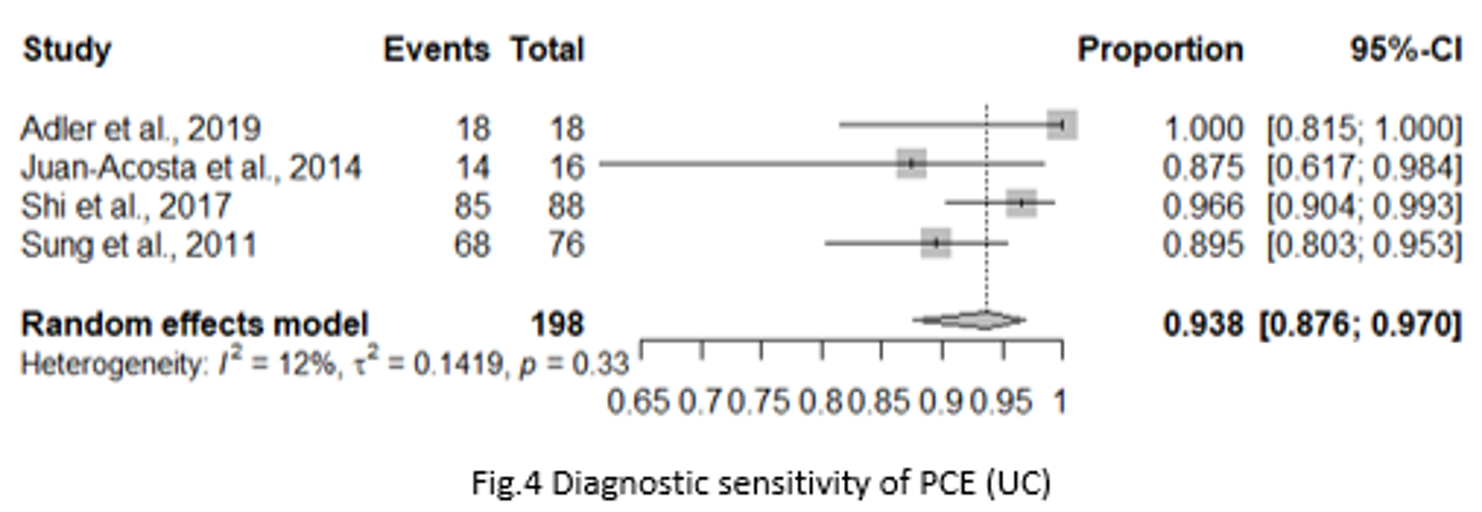
Fourteen studies, including 797 patients, were identified comparing PCE diagnostic yield with colonoscopy or MRE. Seven studies evaluated PCE diagnostic yield in CD and 7 studies in UC. There was a low risk of bias for the majority of included studies; only 1 study was found to have a high risk of bias. In CD, there was a trend to superiority of PCE over MRE and colonoscopy (individually and for pooled outcomes) with a pooled odds ratio (OR) of 1.25 (95% CI 0.85-1.86) (Fig 1) for the detection of CD. This translates to an incremental benefit in diagnostic yield of 5% and 7% for PCE compared with MRE and colonoscopy respectively. PCE performed comparably with colonoscopy in the terminal ileum and colon with ORs of 1.19 (95% CI 0.78-1.79) (Fig 2), and 1.14 (95% CI 0.76-1.71) (Fig 3) respectively. PCEs had a diagnostic sensitivity for the detection of UC of 93.8% (95% CI 87.6%-97.0%) (Fig 4) and a specificity of 69.8% (95% CI, 38.2%-89.6%). This equates to a diagnostic OR of 24.0 (95% CI 10.4-55.3). Subgroup analysis suggested that newer PCEs had greater diagnostic yield than the earlier devices (for UC and CD).


Conclusion
PCEs have a comparable diagnostic yield to colonoscopy and MRE in Crohn’s disease. This was true for the small and large bowel, giving PCE an advantage over standard CE as a single pan-enteric assessment tool for CD. Limitations include the standardisation of PCE scoring systems and the lack of transmural assessment. In UC, PCE has an excellent diagnostic sensitivity and positive predictive value, but is limited by the lack of histologic assessment and poor specificity.


