P205 Impact of histologic disease activity on long-term outcomes in patients with ileal pouch-anal anastomosis for ulcerative colitis
Gabbiadini, R.(1)*;Spaggiari, P.(2);Dal Buono, A.(1);Iuzzolino, M.(2);Furfaro, F.(3);D'Amico, F.(3);Repici, A.(4,5);Spinelli, A.(5,6);Armuzzi, A.(1,5);
(1)Humanitas Research Hospital - IRCCS, IBD Center, Rozzano- Milan, Italy;(2)Humanitas Research Hospital - IRCCS, Department of Pathology, Rozzano- Milan, Italy;(3)Ospedale San Raffaele - IRCCS, Gastroenterology and Endoscopy, Milan, Italy;(4)Humanitas Research Hospital -IRCCS, Department of Gastroenterology, Rozzano- Milan, Italy;(5)Humanitas University, Department of Biomedical Sciences, Pieve Emanuele- Milan, Italy;(6)Humanitas Research Hospital - IRCCS, Division of Colon and Rectal Surgery, Rozzano- Milan, Italy;
Background
Total proctocolectomy with ileal pouch-anal anastomosis (IPAA) for ulcerative colitis (UC) can incur in several complications like pouchitis leading to the need of immunosuppressive therapy, hospitalization and pouch failure. Unlike non-operated UC patients, therapeutic goals are an unmet need in UC-IPAA patients and the impact of the histologic activity on the development of complications is unknown. The aim of the study was to assess the association between histology and the risk of long-term negative outcomes in UC subjects with IPAA.
Methods
This is a single-center, retrospective study which included UC adult patients with IPAA undergoing at least one pouchscopy with biopsies in the pouch body after ileostomy closure. Pouch biopsies were blindly reviewed by a gastrointestinal pathologist with expertise in IBD. Histologic disease remission was defined as a Pouchitis Disease Activity Index (PDAI) histology subscore £ 1. Negative outcomes were: IPAA related complications (acute or chronic pouchitis, hospitalization, pouch failure) and escalation of medical therapy (start of immunosuppressive or biologics). Both descriptive and inferential statistical analyses carried out
Results
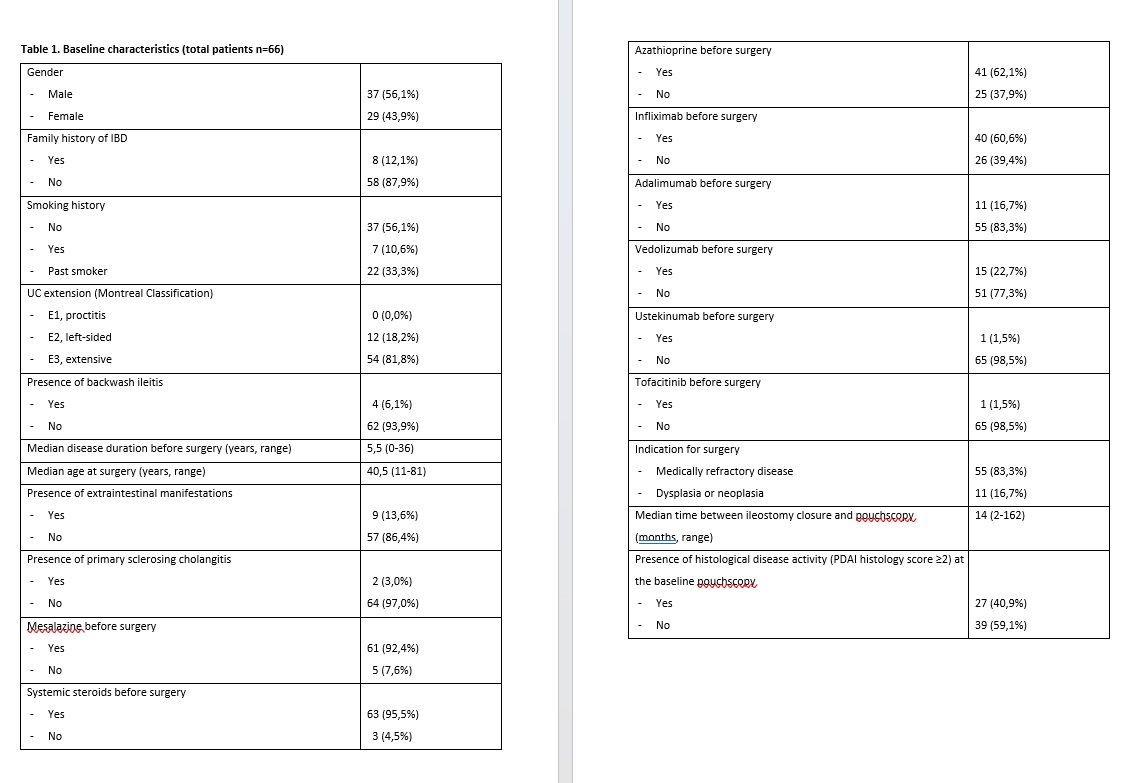
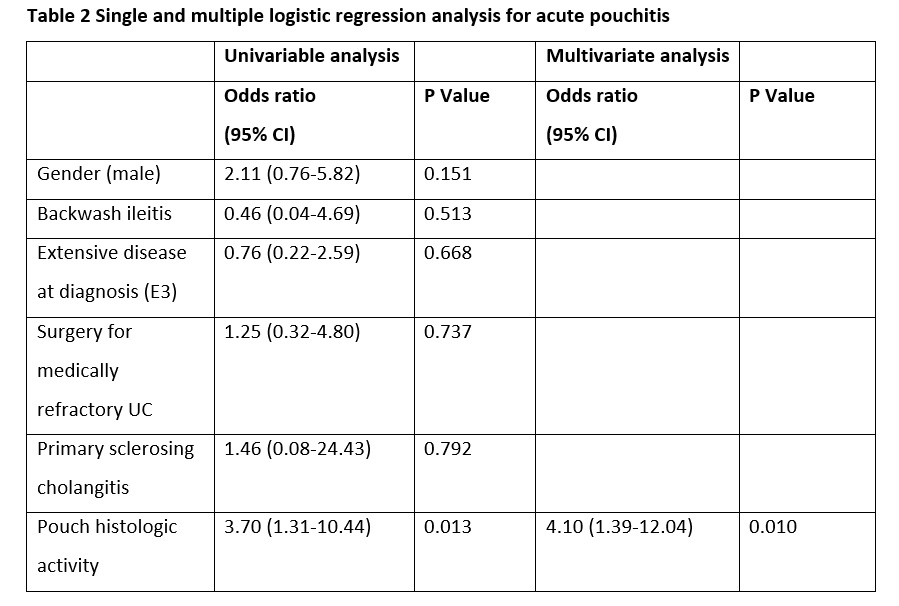
A total of 66 patients were included (male n=37; 56,1%) of whom 40,9% (n=27) had histological activity at the baseline pouchscopy. The characteristics of the study population are represented in table 1. The median time of follow up was 38,5 months (range 12-151). During the study period, 27 patients (40,9%) developed acute pouchitis and 10 patients (15,2%) chronic pouchitis. Thirty-nine subjects (59,1%) required antibiotic therapy while 8 subjects required systemic steroids (12,1%). Furthermore, 15 patients (22,7%) started immunomodulatory therapy with either azathioprine or biologic agents. Six patients (9,1%) needed pouch-related hospitalization and 1 patients (1,5%) experienced pouch failure. Chronic pouchitis and the need of immunosuppressive/biology therapy was observed more frequently in patients with pouch histologic activity (29,6% vs. 5,1%, and 40,7% vs. 10,3%, respectively) (P<0.05). After adjusting for risk factors for pouchitis, the presence of histologic activity remained an independent risk factor for developing acute pouchitis (OR 4.10, 95% CI 1.39-12.04; P= 0.010), chronic pouchitis (OR 8.51, 95% CI 1.51-47.80, P=0.015) and the need for immunosuppressive or biologic therapy (OR 6.98, 95% CI 1.69-28.80; P=0.007).

Conclusion
Histologic activity was associated with an increased risk of developing both acute and chronic pouchitis and with the need for immunosuppressive/biologic therapy. Future research will clarify whether histologic remission might be considered as a therapeutic target for UC-IPAA patients developing pouchitis.


