P240 Low surgery rates first year after diagnosis in Crohn’s disease; results from a large population-based inception cohort - the IBSEN III study
Lund, C.(1,2)*;Strande, V.(2,3,4);Småstuen, M.C.(1,5);Bengtson, M.B.(6);Cetinkaya, R.B.(7);Detlie, T.E.(2,8);Frigstad, S.O.(9);Medhus, A.W.(1,2);Henriksen, M.(10);Holten, K.I.A.(2,10);Hovde, Ø.(2,11);Huppertz-Hauss, G.(12);Johansen, I.(13,14);Olsen, B.C.(2,12);Opheim, R.(1,14);Pallenschat, J.(15);Perminow, G.(16);Ricanek, P.(4,8);Vatn, S.(8);Aabrekk, T.B.(2,6);Kristensen, V.A.(1,3);Høivik, M.L.(1,2);
(1)Oslo University Hospital, Department of Gastroenterology, Oslo, Norway;(2)University of Oslo, Institute of Clinical Medicine, Oslo, Norway;(3)Unger-Vetlesen Institute, Lovisenberg Diaconal Hospital, Oslo, Norway;(4)Lovisenberg Diaconal Hospital, Department of Gastroenterology, Oslo, Norway;(5)Oslo Metropolitan University, Department of Public Health, Oslo, Norway;(6)Vestfold Hospital Trust, Department of Gastroenterology, Tønsberg, Norway;(7)Diakonhjemmet Hospital, Department of Medicine, Oslo, Norway;(8)Akershus University Hospital, Department of Gastroenterology, Lørenskog, Norway;(9)Vestre Viken Hospital Trust- Bærum Hospital, Department of Internal Medicine, Gjettum, Norway;(10)Østfold Hospital Trust, Department of Gastroenterology, Sarpsborg, Norway;(11)Innlandet Hospital Trust, Department of Internal Medicine, Gjøvik, Norway;(12)Telemark Hospital Trust, Department of Gastroenterology, Skien, Norway;(13)Østfold University College, Faculty of Health- Welfare and Org., Fredrikstad, Norway;(14)University of Oslo, Institute of Health and Society - Department of Public Health, Oslo, Norway;(15)Sørlandet Hospital- Flekkefjord, Department of Internal Medicine, Flekkefjord, Norway;(16)Oslo University Hospital, Department of Paediatrics, Oslo, Norway;
Background
Surgery rates in Crohn’s disease (CD) have declined during recent years, in parallel with the introduction and increased use of biological treatment. The aim of this study was to describe the use of first-line biologic therapy and to estimate the intra-abdominal surgery rate during the first year after the CD diagnosis.
Methods
The Inflammatory Bowel Disease in South-Eastern Norway III (IBSEN III) study is a population-based inception cohort with a prospective follow-up of newly diagnosed inflammatory bowel disease patients from the South-Eastern Health Region of Norway included in the period 2017 to 2019. Five hundred and seven patients ≥18 years were diagnosed with CD and those attending the one-year follow-up visit were included in this study. Clinical data, including Montreal classification, were registered at time of diagnosis. At the one-year follow-up, use of biologic therapy and need for CD-related intra-abdominal surgery since diagnosis were registered. Kaplan-Meier plots estimated the cumulative incidence of first-line biologic therapy and intra-abdominal surgery.
Results
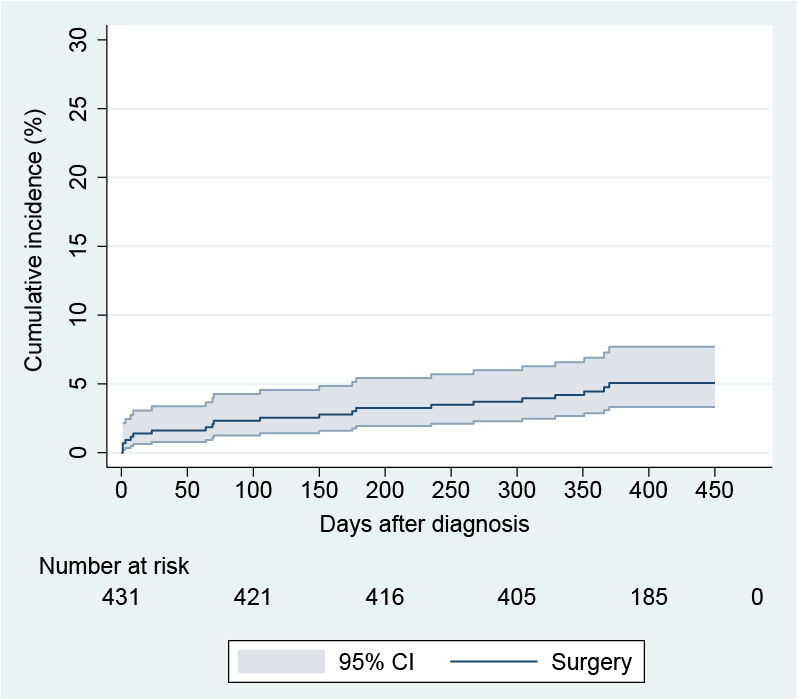
A total of 431/507 (85%) CD patients attended the one-year follow-up and were included, 54.8% female, median age 37 years (range 18-80). At diagnosis 218 (50.6%) presented with ileal disease location, 76 (17.6%) colonic and 137 (31.8%) ileocolonic disease location, while 11 (2.6%) also had upper gastrointestinal involvement. The majority, 351 (81.4%), had a non-stricturing non-penetrating disease behavior, 70 (16.2%) a stricturing and 10 (2.3%) a penetrating disease behavior, while 17 (3.9%) also had perianal disease. Within one year of follow-up, 165 (38.7%) received at least one biologic therapy (60.6% infliximab, 35.8% adalimumab and 3.6% vedolizumab). Seven patients (1.6%) underwent perianal surgery and 21 (4.9%) had intra-abdominal surgery within the first year. Three of these were diagnosed during their primary surgery. Time from diagnosis to start of first-line biologic therapy and first intra-abdominal surgery is shown in Figure 1 and Figure 2, respectively.
Conclusion
In the IBSEN III cohort, the rate of intra-abdominal surgery during the first year of disease was low (4.9%) compared to a previous population-based study from the same geographic area during the pre-biologic era, the IBSEN study, where the surgery rate was reported as 15.9 %.1 We hypothesize that a large preponderance of patients presenting with milder phenotypes at diagnosis combined with high use of biologicals contribute to the low surgery rates.
Figure 1: Kaplan-Meier plot showing cumulative incidence of first-line biologic therapy.
Figure 2: Kaplan-Meier plot showing cumulative incidence of Crohn's related intra-abdominal surgery.