P250 The impact of Primary Sclerosing Cholangitis (PSC) on fecal calprotectin assessment in individuals with Inflammatory Bowel Disease (IBD)
Arar, A.(1);Scott, F.(2);Click, B.(2);Fennimore, B.(2);Ahmed, W.(2);Oonk, A.(2);Gerich, M.(2)*;
(1)University of Colorado Anschutz Medical Campus, Department of Medicine, Aurora, United States;(2)University of Colorado Anschutz Medical Campus, Division of Gastroenterology & Hepatology, Aurora, United States;
Background
Fecal calprotectin (FCP) is recommended as a non-invasive biomarker in ulcerative colitis (UC); however, the accuracy of FCP in individuals with concurrent primary sclerosing cholangitis (PSC) is less understood due to biliary fluid calprotectin excretion in PSC. We aimed to determine the relationship of endoscopic disease activity to FCP levels in individuals with PSC and colitis (PSC-IBD) compared to individuals with UC alone.
Methods
Individuals with PSC-IBD and UC controls who underwent colonoscopy at a large tertiary academic medical center. Controls with similar UC extent were selected in a 2:1 ratio. Mayo endoscopic scores (MES) were derived from the endoscopic database. If no prospective score was recorded, images were reviewed by two investigators with adjudicated discrepancies. Disease characteristics, baseline demographics, FCP (within 6 months of endoscopy), and C-reactive protein (CRP) were derived from the electronic medical record. Exclusion criteria included Crohn's disease or non-IBD colitis, infectious colitis, treatment change between endoscopy and FCP measurement, and colonic resection. Mean FCPs and standard deviations (SDs) were calculated, stratified by PSC status and MES. Multivariable linear regression was employed to assess the association of PSC on FCP adjusting for MES, age, alkaline phosphatase (ALP), and disease location.
Results
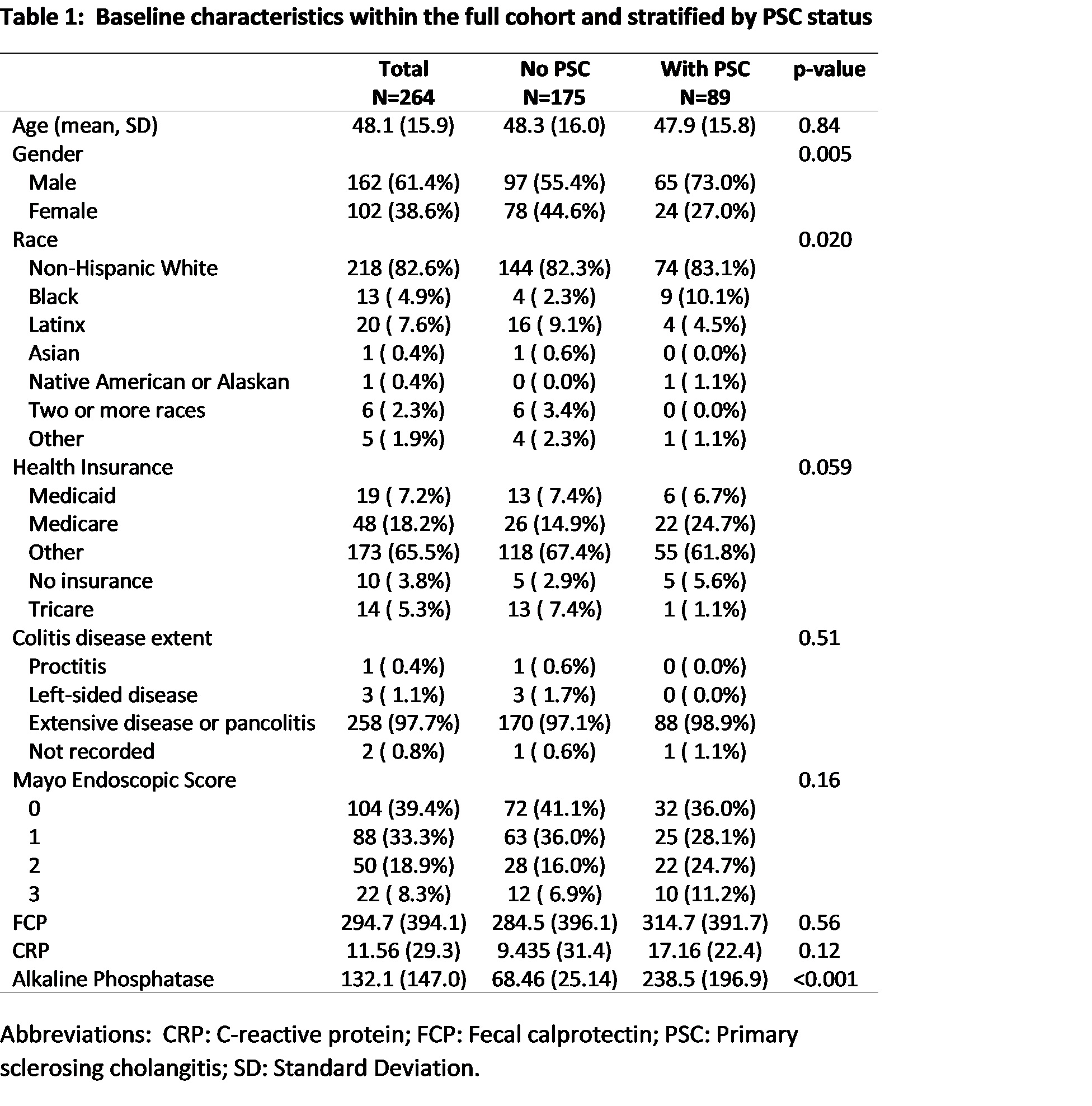
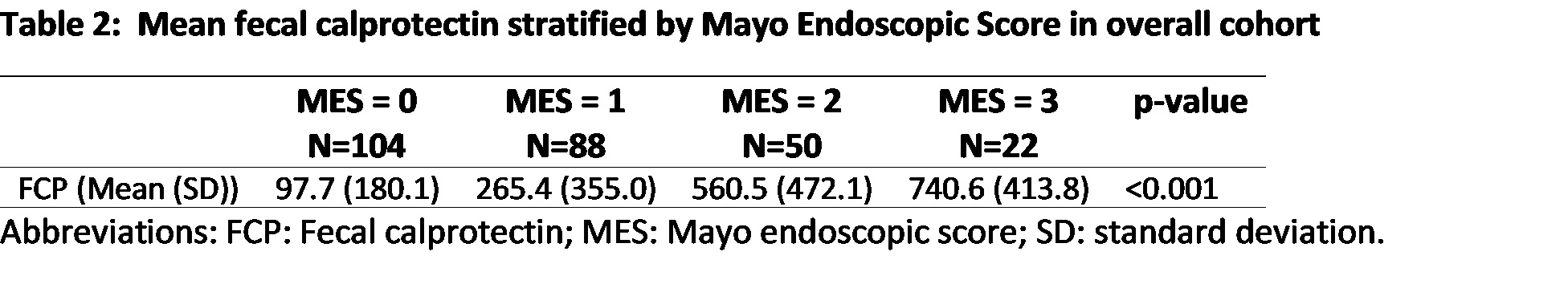
264 colonoscopies for 197 patients (mean age 48, 61% males, 97% extensive disease) were identified with corresponding FCP from 2013 to 2022. Compared to UC controls, there were more males in the PSC-IBD cohort; MES did not differ significantly between the two groups (Table 1). There was no significant difference in mean FCP in PSC-IBD compared to UC controls (314.7 vs 284.5, p=0.56). Mean FCP increased with increasing MES (Table 2). There was no significant difference in mean FCP between those with PSC and those without when stratified by MES (Table 3). In multivariable linear regression, left-sided disease extent, MES, and ALP were independently associated with increasing FCP (Table 4).


Conclusion
In this cohort, a diagnosis of PSC was not associated with significant differences in FCP for IBD patients when stratified by MES. These data suggest that FCP remains a reliable marker of colitis activity in IBD patients with and without PSC. Further research is required to understand the role of PSC activity in modulating FCP concentrations.


