P267 Milan Ultrasound Criteria are accurate in assessing endoscopic remission and treatment response in patients with ulcerative colitis
Allocca , M.(1);Dell'Avalle , C.(2);Radice , S.(3);Furfaro , F.(4);Zilli , A.(3);D'Amico , F.(3);Peyrin-Biroulet , L.(5);Fiorino , G.(3);Danese , S.(3);
(1)IRCCS San Raffaele Scientific Institute, Gastroenterology and Gastrointestinal Endoscopy Unit, Milan, Italy;(2)Humanitas University, Biomedical Science, Pieve Emanuele, Italy;(3)IRCCS Ospedale San Raffaele and Vita-Salute University San Raffaele, Gastroenterology and Digestive Endoscopy, Milan, Italy;(4)Humanitas Research Hospital, Gastroenterology, Rozzano, Italy;(5)University Hospital of Nancy- University of Lorraine, Gastroenterology and INSERM NGERE 1256, Nancy, France;
Background
We assessed the accuracy and the responsiveness to change of Milan Ultrasound Criteria (MUC) in patients with ulcerative colitis (UC), using colonoscopy as the reference standard.
Methods
We performed a prospective observational study of 49 patients with active UC. All patients underwent bowel ultrasound and colonoscopy at baseline and at reassessment, at week 48, after treatment with biologics (29 patients were treated with infliximab, 14 with vedolizumab, four with adalimumab, two with ustekinumab). Furthermore, patients underwent bowel US also at week 12 and 24. Disease activity was quantified using Mayo endoscopic subscore and MUC. The primary analysis was to determine the accuracy of MUC in identification of endoscopic remission defined as a Mayo endoscopic subscore < 2. Additional analyses established the accuracy of MUC in determining change in lesion severity. Logistic regression was used to examine the relationship between the absence or presence (0/1) of endoscopic remission at reassessment as the dependent variable and possible predictors at week 12 as the independent variables. The model was performed using the stepwise backward method.
Results
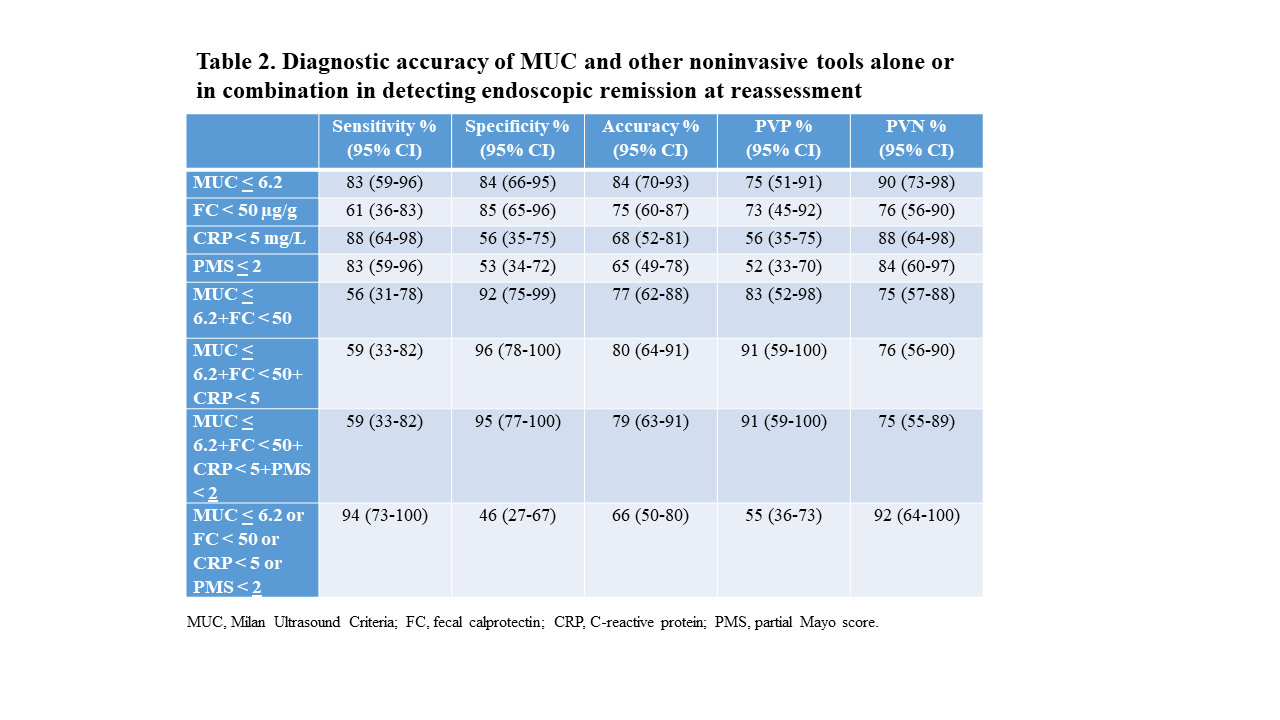
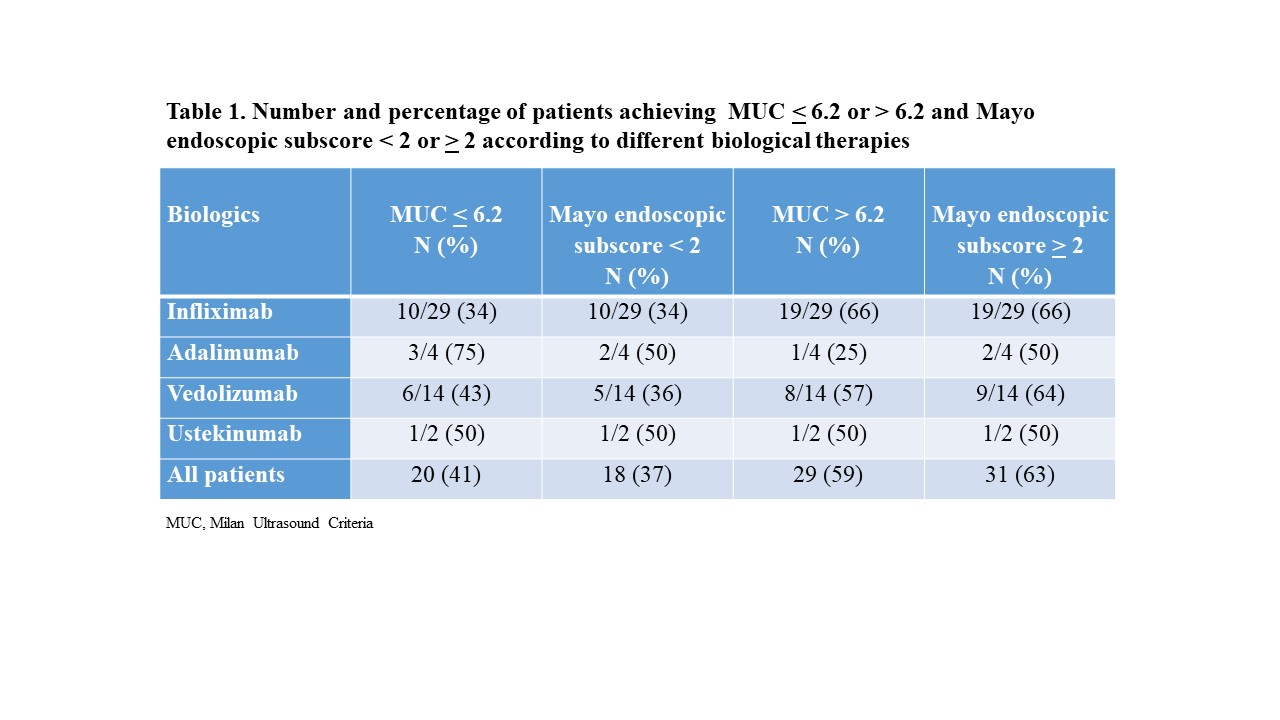
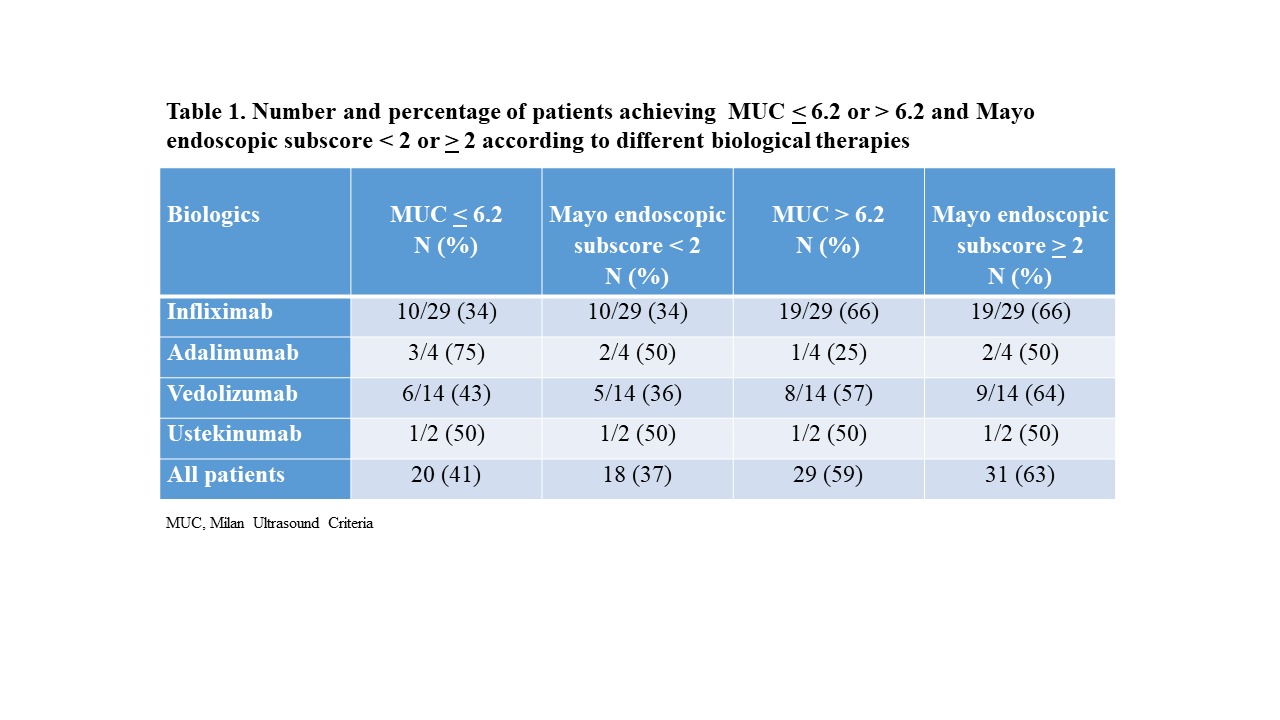
Eighteen patients (37%) got endoscopic remission at reassessment. In Table 1 are summarized endoscopic and ultrasound outcomes achieved at reassessment according to the different treatments. MUC < 6.2 determined endoscopic remission with 83% sensitivity, 84% specificity, 84% accuracy, 75% PVP and 90% PVN (Table 2). MUC was sensitive to change in ulcerative colitis [Guyatt’s responsiveness index: 1.73; standardised effect size ratio: 2.0]. MUC changed significantly from baseline to reassessment [8.72 (7.78−9.14) vs 7.60 (4.71−8.53), p < 0.0001], with the largest drop at week 12 [8.72 (7.82−9.19) vs 7.46 (5.80−7.98), p < 0.0001] (Figure 1). A change of -2 in MUC overtime predicted endoscopic remission at reassessment (AUC 0.806, 95% CI 0.667-0.904; sensitivity 89%, specificity 77%). At multivariable analysis only MUC < 6.2 at week 12 was statistically significantly associated with endoscopic remission at reassessment (Table 3).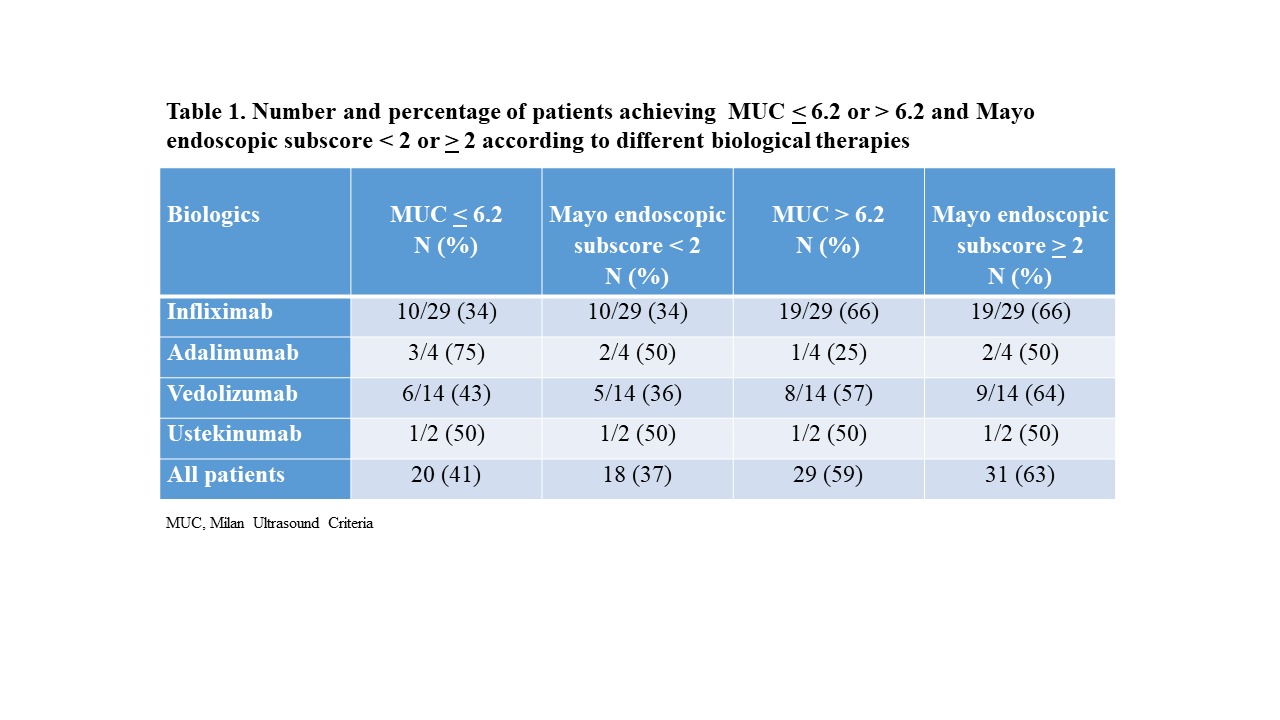






Conclusion
MUC accurately detects endoscopic remission. MUC is a highly responsive, reliable tool for assessing treatment response in patients with ulcerative colitis.


