P309 Accuracy of PanMayo endoscopic score in predicting long-term disease outcomes in ulcerative colitis– a promising scoring system
Bacsur, P.(1)*;Wetwittayakhlang, P.(2);Resál, T.(1);Rutka, M.(1);Bessissow, T.(2);Atif, W.(2);Bálint, A.(1);Fábián, A.(1);Bor, R.(1);Szepes, Z.(1);Farkas, K.(1);Lakatos, P.L.(2,3);Molnár, T.(1);
(1)Szent-Györgyi Albert Medical School- University of Szeged, Department of Medicine, Szeged, Hungary;(2)McGill University Health Center, Division of Gastroenterology, Montreal, Canada;(3)Semmelweis University, Department of Oncology and Medicine, Budapest, Hungary;
Background
Ulcerative colitis (UC) is a systemic immune-mediated disease that affects the colon continuously. Colonoscopy plays a crucial role in management of UC that helps to assess mucosal healing objectively along the colon. Different scoring systems are available to assess severity, however most of them does not take into consideration of disease extent. Extension modified (PanMayo) Mayo endoscopic subscore (MES) system has been shown to correlate with UCEIS and Riley scores and calprotectin. Our study aimed to assess the predictive power and accuracy of PanMayo score compared to MES, UCEIS and Dublin to predict mid- and long-term disease outcomes.
Methods
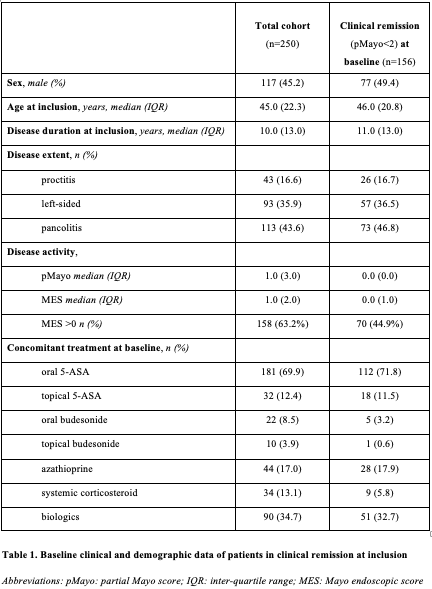
This is retrospective, two-center study. UC patients, who underwent colonoscopy due to any reason between 2016 and 2018, were consecutively enrolled. PanMayo, MES, UCEIS and Dublin scores and additionally the Nancy histology score (where available) were recorded with clinical and demographical data at baseline. Disease flare, need for change in therapy (incl. initiation of biologicals, need for systemic steroids), hospitalisations and colectomy were tracked amongst patients with clinical remission (pMayo<2) during an at least 3-years follow-up to assess predictive value of score systems. Log-rank, Cox regression analysis and Chi2 tests were used to analyse outcomes and Kaplan Meier curves were plotted.
Results
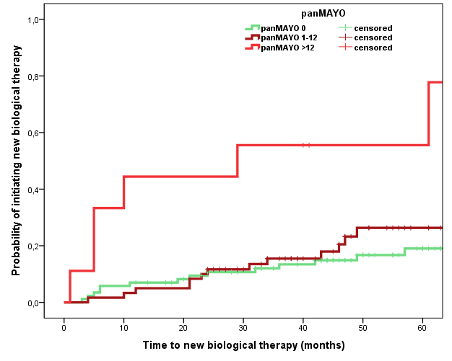
A total of 250 UC patients (male ratio: 0.45, median age 45 (IQR) 22.3 years) were enrolled with 156 (male ratio 0.49; mean age 46 IQR 20.8 years, Table 1.) of UC patients having baseline clinical remission. PanMayo, MES, and Dublin scores were positively associated with risk of disease flare (Figure 1.; p=0.002, p<0.01, p=0.003). Increasing MES score was coupled with risk of relapse (MES0=26.7%, MES1=53.1% and MES2-3=47.6%; p=0.008). PanMayo score (above 12 points), but not MES or UCEIS, was associated with the need of new biological (Figure 2.; 66.7% vs. 21.7%; p<0.001) and treatment escalation (33.3 vs. 11.5%; p=0.018), similar trend was found for the Dublin score for need for new biologicals. There was a strong trend for PanMayo to predict need for hospital admission (p=0.06). All scores were strongly associated with need for systemic corticosteroids. Colectomy rates were low. Nancy score showed only a trend to predict risk of clinical flare and need for corticosteroids.
Conclusion
Our study suggests that combined endoscopic assessment of the extent and severity may be more accurate in predicting disease outcomes in UC in clinical remission. PanMayo scores may be an alternative of the existing scoring system and was associated more granularly with disease outcomes. In addition, outcomes were different in patients with initial MES 0 and 1 scores.


