P397 Can upskilling pharmacy technicians support a robust and cost-effective Inflammatory Bowel Disease patient review process? A single-centre prospective study.
Rees, F.(1);Packham, A.(1);St Clair Jones, A.(1);Smith, M.(1);
(1)University Sussex Hospitals NHS Foundation Trust, IBD Team- Gastroenterology, Brighton, United Kingdom;
Background
Immunomodulators are key to the management of Inflammatory bowel disease (IBD). To ensure safety and efficacy, UK guidance recommend immunomodulator review.
At University Hospitals Sussex (UHS), reviews are completed by a multi-disciplinary team (MDT), with specialised IBD pharmacists and nurses leading on autonomous blood monitoring and symptom review (figure 1).
This workload puts considerable strain on the UHS IBD team. Upskilling and task shifting is recognised as legitimate strategy for service enhancement, care access, cost effectiveness and sustainability plus ensures team flexibility, boosted morale and career progression.
The UHS IBD team includes a highly motivated pharmacy technician (PT). In the UK, PT are registered non-prescribing healthcare professionals, but training does not include autonomous blood monitoring and symptom review.
Methods
To ensure competency of autonomous blood monitoring and symptom review, a training package was developed and was approved by UHS Medicines Governance Group.
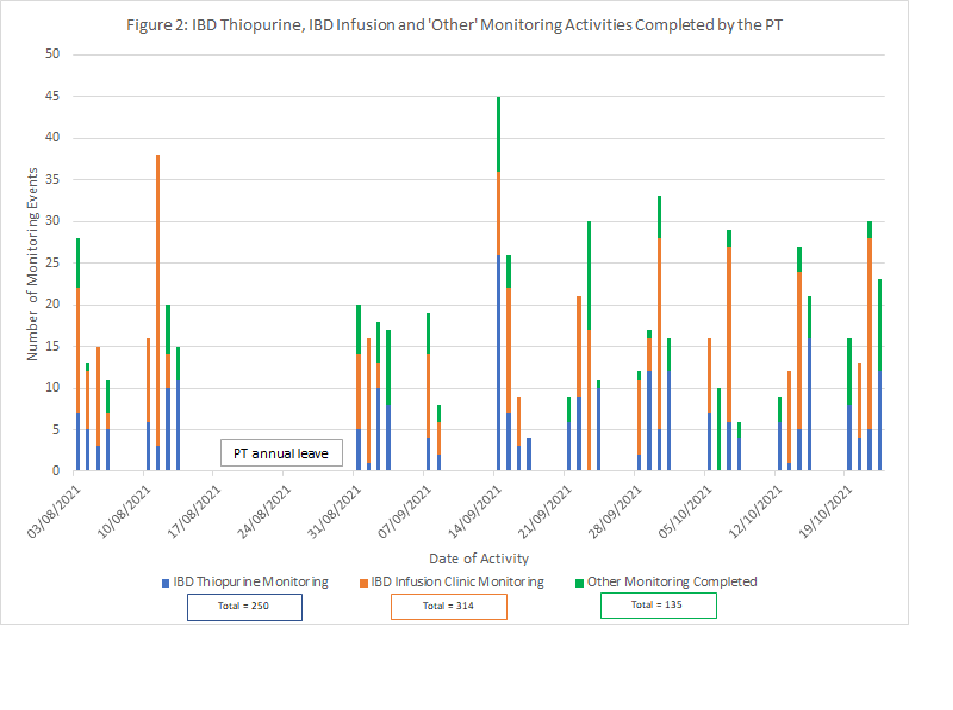
Once accredited, PT prospectively recorded blood monitoring and symptom review activity over 10-weeks (figure 2 and 3) and referrals completed (figure 4).
Results
The training package was completed in 10 weeks.
Over 10 weeks, PT completed 699 distinct monitoring activities, with 57 (8%) needing referral to the specialised pharmacist.
The highest proportion of workload was observed in the IBD infusion clinic (314, 45%), followed by thiopurine monitoring (250, 36%) and then ‘others’ (135, 19%). ‘Others’ were essential IBD activities including faecal calprotectin levels (FCPL), pre-initiation tests (e.g. thiopurine methyltransferase levels (TPMT), viral screening, t-spots) and medication levels to optimise therapy.
All referrals to the specialised pharmacist were appropriate as needed action by a prescribing professional.
In addition, PT contributed substantially to data collection for virtual biologic clinic (VBIC) reviews; 32 patients.
Feedback has been overwhelmingly positive from all effected stakeholders (PT, IBD pharmacy and nursing team and gastroenterologists).


Conclusion
Identifying appropriate tasks and upskilling the IBD PT has enabled a more cost-effective and efficient use of IBD workflow, care standardisation, team robustness and staff morale.
Approved training and support are required to enable upskilling and continued service safety and we recommend that skills are recognised locally and nationally.


