P413 Characteristics of the stricture, not the ongoing treatment, influence the outcome of endoscopic dilatation in recurrent Crohn`s disease.
Ladrón Abia, P.(1); Alonso, N.(2);Beltrán, B.(1);Minguez, A.(1);Sáez-González, E.(1);Pons-Beltrán, V.(2);Nos, P.(1);Iborra, M.(1);
(1)Hospital Universitari i Politècnic La Fe, Gastroenterology Unit- Digestive Diseases Department, Valencia, Spain;(2)Hospital Universitari i Politècnic La Fe, Gastrointestinal Endoscopy Unit- Digestive Diseases Department, Valencia, Spain
Background
Endoscopic balloon dilatation (EBD) is a conservative alternative for the treatment of post-surgical anastomotic strictures in Crohn's disease (CD) that improves obstructive symptoms and could delay or avoid further surgeries. However, the usefulness of this technique and predictors of efficacy have been poorly evaluated in a homogeneous cohort. Aim: to evaluate the efficacy of EBD in CD patients with anastomotic strictures as well as to analyze therapeutic success factors and the rate of adverse events.
Methods
Observational study in a tertiary hospital of a cohort of patients with diagnosis of CD who underwent EBD for anastomotic stricture after previous surgery and with obstructive symptoms. Clinical, demographic and disease characteristics, treatment used, surgery data, inflammatory parameters at time of dilatation, number of dilatations, complications and needed for subsequent surgery were analyzed. Technical success was defined when the endoscope was passed through the stricture after procedure. Therapeutic success per patient was considered when patient did not need surgery at the end of the follow-up.
Results
63 EBD were performed in 32 patients. Figure 1 shows the clinical and demographic characteristics of the patients. The diameters of the balloons used were 12-15 mm and 15-18 mm. Of the 63 examinations performed, 63.5% (n=40) showed technical success. The therapeutic success per patient was 62.5% (n=20) at 6 years of mean follow-up. Twelve patients required new surgery. The visualized neoileon after EBD had no significant recurrence (Rutgeerts i0-i2a) in 80% of dilatations. The adverse event rate was 3.1% (n=2) a microperforation and a major bleeding, both patients with Rutgeerts i4. The stricture length was the only predictor of technical and therapeutic success. Strictures with more than 40 mm of length were associated with poor efficacy. Neither the type of surgical anastomosis, current treatment, inflammatory parameters levels or balloon diameter were predictors of therapeutic success.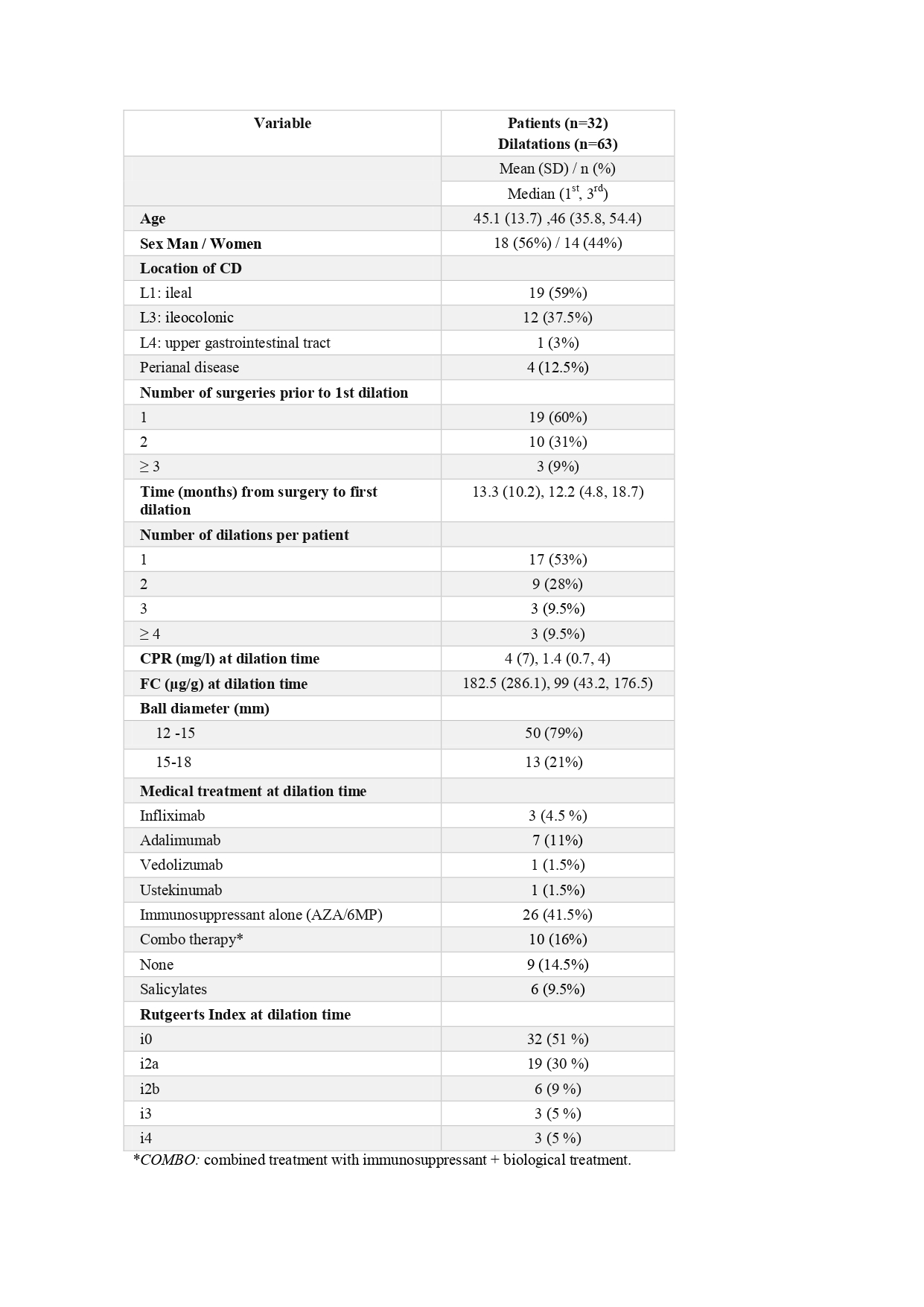
Conclusion
EBD appears to be a safe and effective technique that could avoid further surgery in up to two thirds of anastomotic strictures in CD in long-term recurrent CD. Longer stricture length and the presence of severe recurrence were associated with poor response and complications.


