P413 Withdrawal versus continuation of thiopurine in vedolizumab-treated patients with Ulcerative Colitis (VIEWS): a multi-centre randomised controlled trial
Pudipeddi, A.(1)*;Paramsothy, S.(1);Kariyawasam, V.(2);Paramsothy, R.(2);Ghaly, S.(3);Haifer, C.(3);An, Y.K.(4);Begun, J.(4);Connor, S.(5);Corte, C.(6);Ward, M.(7);De Cruz, P.(8);Fung, C.(9);Redmond, D.(1);Leong, R.W.(1);
(1)Concord Repatriation General Hospital, Department of Gastroenterology and Hepatology, Sydney, Australia;(2)Blacktown Hospital, Department of Gastroenterology, Sydney, Australia;(3)St Vincent's Hospital, Department of Gastroenterology, Sydney, Australia;(4)Mater Hospital, Department of Gastroenterology, Brisbane, Australia;(5)Liverpool Hospital, Department of Gastroenterology, Sydney, Australia;(6)Royal Prince Alfred Hospital, AW Morrow Gastroenterology and Liver Centre, Sydney, Australia;(7)The Alfred Hospital, Department of Gastroenterology, Melbourne, Australia;(8)Austin Hospital, Department of Gastroenterology, Melbourne, Australia;(9)Concord Repatriation General Hospital, Department of Anatomical Pathology, Sydney, Australia;
Background
The benefit of continuing thiopurine in ulcerative colitis (UC) responders to vedolizumab (VED) is unclear. We aimed to determine the effect of thiopurine withdrawal in VED-treated UC patients on combination therapy.
Methods
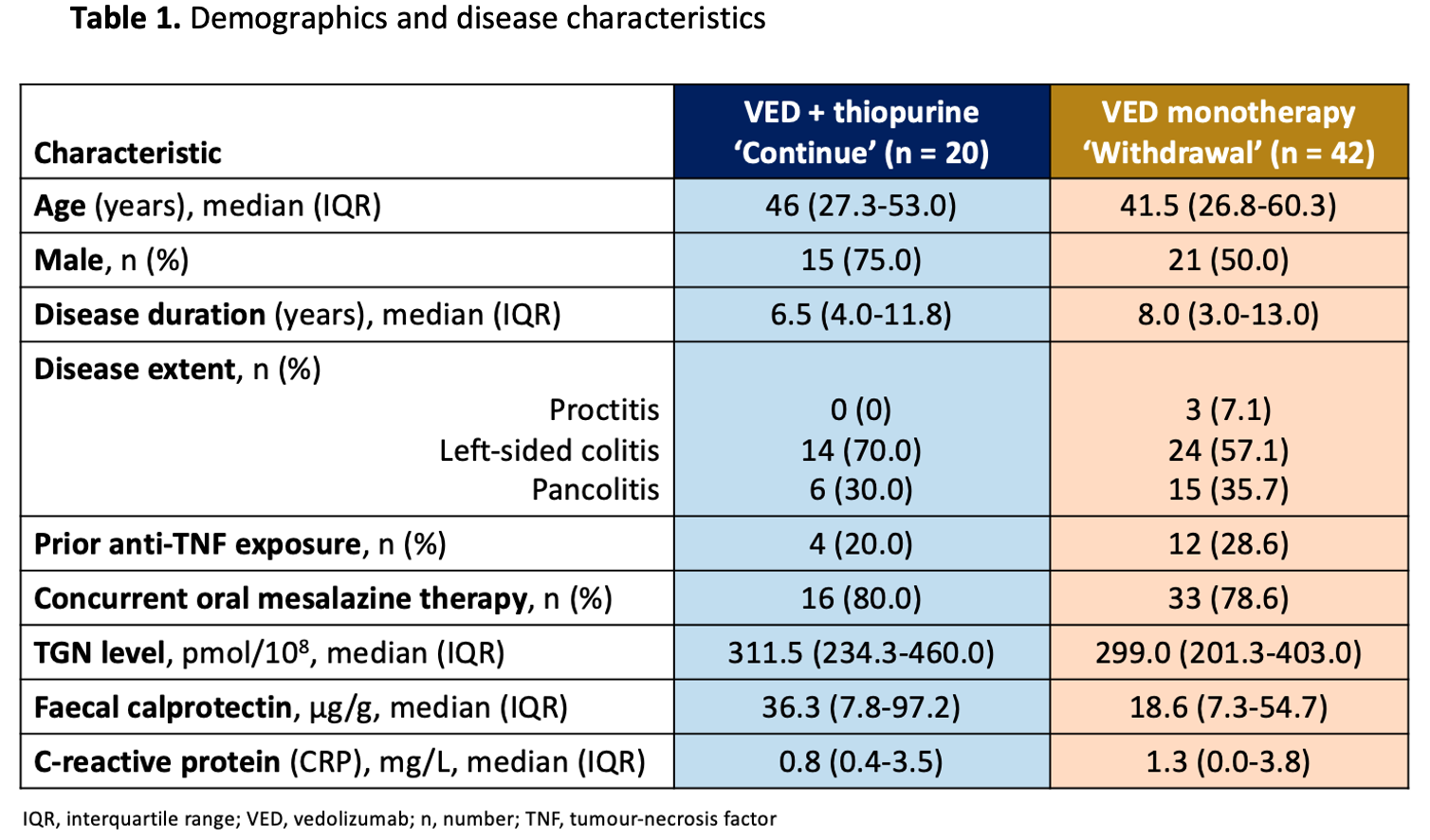
This prospective multi-centre, single-blind, randomised controlled trial recruited UC patients on VED 300mg IV every 8 weeks and a thiopurine for ≥6 months. Patients in steroid-free clinical remission (partial Mayo score[pMS]≤2, no subscore>1) and endoscopic remission/improvement (Mayo endoscopic subscore[MES]≤1) were randomised 2:1 to withdraw or continue thiopurine. Primary outcome was comparing week 48 VED trough levels. Secondary outcomes were disease relapse (pMS≥3 and faecal calprotectin>150μg/g or increase in MES≥1 from baseline), centrally-read endoscopic remission (MES=0), histologic remission (Nancy index=0), histo-endoscopic remission, faecal calprotectin (remission<150μg/g) and adverse events.
Results
Sixty-two consecutive patients (58% males, median follow-up 23.0 months) were randomised to withdraw (n=42) or continue (n=20) thiopurine. Randomisation was balanced. Complete data was available for 58 patients. There was a non-significant trend toward increased disease relapse in the withdrawal group (P=0.12, Fig. 1). In the withdrawal group, baseline histologic activity significantly increased disease relapse (HR:5.8, 95%CI:1.6-20.8, P=0.007, Fig. 2). There was a trend towards higher relapse rates in the withdrawal versus continue groups for bio-exposed patients (50.0% [6/12] vs 0.0% [0/4], P=0.07) but not bio-naïve patients (20.0% [6/30] vs 12.5% [2/16], P=0.52). At week 48, the continue group had significantly higher histologic remission (OR:4.6, 95%CI:1.1-18.9, P=0.03) and histo-endoscopic remission rates (OR:4.6, 95%CI:1.3-16.1, P=0.01, Fig. 3) versus the withdrawal group, but similar endoscopic remission rates (P=0.09, Fig. 3). Faecal calprotectin remission was significantly higher in the continue (94% [16/17]) versus withdrawal group (70% [28/40], P=0.047) with mean calprotectin 44.5μg/g±SD56.2 vs 209.6μg/g±SD344.2 (P=0.003) respectively. On multivariate analysis, histologic activity at baseline (HR:5.3, 95%CI:1.1-26.2,P=0.04) predicted disease relapse. Week 48 median VED levels were 15.9µg/mL (IQR:10.1-22.7) in the withdrawal group versus 14.7µg/mL (IQR:12.1-18.7) in the continue group (P=0.43). No patients had anti-VED antibodies. There was no significant difference in adverse events between groups.
Conclusion
Although thiopurine withdrawal did not affect VED trough level, it increased calprotectin, histologic and histo-endoscopic activity in UC. In patients with histological activity despite deep remission, thiopurine withdrawal significantly increased the risk of disease relapse.