P425 The utility of intestinal ultrasound to inform clinical decision making
Yeaman, F.(1)*;Panaccione, R.(1);Ma, C.(1);Lu, C.(1);Seow, C.(1);Kaplan, G.(1);Maracle, B.(1);Novak, K.(1);
(1)University of Calgary- Foothills Medical Centre, Gastroenterology and Hepatology, Calgary, Canada;
Background
Inflammatory bowel disease (IBD) is a chronic, immune-mediated disease leading to progressive bowel damage. Objective monitoring is essential to improve outcomes. Intestinal ultrasound (IUS) is an accurate, repeatable modality preferred by patients. The aim of this study was to evaluate changes in medical therapy and further tests requested, when IUS is used routinely to follow patients in an expert centre.
Methods
This is a single centre, prospective observational cohort study. All recruited provided informed consent with ethics approval through the University of Calgary. Patients over the age of 18 years were recruited via convenience sampling from October 1, 2020 to September 31, 2022. Patients were part of a registry where clinic-based IUS is standard of care. Patient demographics, medical treatment changes and further investigations were recorded.
IUS were performed by an IBD gastroenterologist trained in advanced IUS. Patients were classified as symptomatic (Harvey Bradshaw Index [HBI] ≥5) or asymptomatic (HBI<5). IUS were categorised as inactive if the bowel wall thickness (BWT) was <3mm without colour Doppler and inflammatory mesenteric fat) or active (BWT ≥3mm, colour Doppler ≥2 and presence of inflammatory fat). Data were reviewed regarding management: medication changes were defined as dose change, addition of corticosteroids or other medication and medication change. Referral for surgical opinion was recorded. Further outcomes included faecal calprotectin, stool for infection, blood tests, endoscopy, imaging or hospital admission.
Results
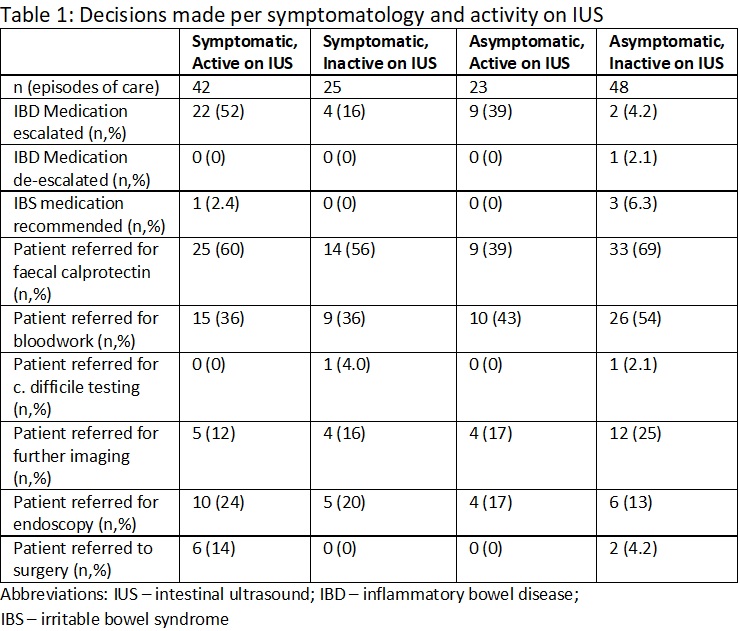
138 episodes of care were logged including 103(74%) with Crohn’s disease, 16(12%) with ulcerative colitis, 2(1.4%) with IBD-unclassified, 13(9.4%) without IBD investigated for symptoms and 4(2.9%) not recorded. Figure 1 shows symptomatic and active episodes compared to asymptomatic and inactive. IUS were performed: for flare symptoms in 22(16%); for monitoring in 107(78%); or to investigate symptoms in 9(6.5%). IBD medication was escalated in 22(52%) patients with active IUS disease plus symptoms and in 9(39%) asymptomatic patients with active IUS. Medication escalation was performed in 4(16%) symptomatic patients with inactive IUS and 2(4.2%) asymptomatic patients with inactive IUS based on low drug level or adverse events. One patient had medication reduced in frequency due to the IUS findings(Table 1). No hospital admissions occurred following IUS.
Conclusion
Active IUS triggered treatment modification in almost 40% of patients, regardless of symptoms. Future studies will assess benefits of timely treatment changes for long term outcome. IUS supports a clinician at the bedside to make timely clinical decisions that may avoid invasive testing and decrease resource limited endoscopy.


