P502 Tumour necrosis factor antagonists are superior to anti-integrin and anti-IL-12/23 therapies for preventing postoperative recurrence in adult Crohn’s disease patients requiring postoperative therapy
T. Nakamura1, R. Shah2, M. Sachs3, S. Chang4, D. Hudesman4, B. Click5, J. Axelrad4
1New York University Medical Center, Medicine, New York, USA, 2Cleveland Clinic Medical Center, Medicine, Cleveland, USA, 3Karolinska, Clinical Epidemiology, Solna, Sweden, 4Gastroenterology and Hepatology, New York University Medical Center, New York, USA, 5Gastroenterology- Hepatology- and Nutrition, Cleveland Clinic Medical Center, Cleveland, USA
Background
Crohn’s disease (CD) recurrence is common after surgical resection. Prior data have demonstrated that postoperative tumour necrosis factor antagonists (anti-TNF) may reduce recurrence, although little is known about the efficacy of other biologic therapies. The aim of this study was to compare biologic type and timing for preventing postoperative objective recurrence in adult CD patients.
Methods
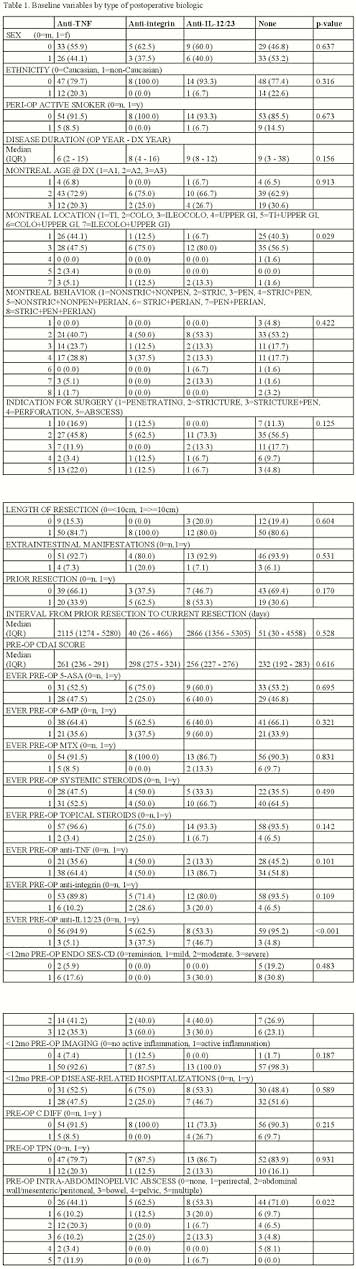
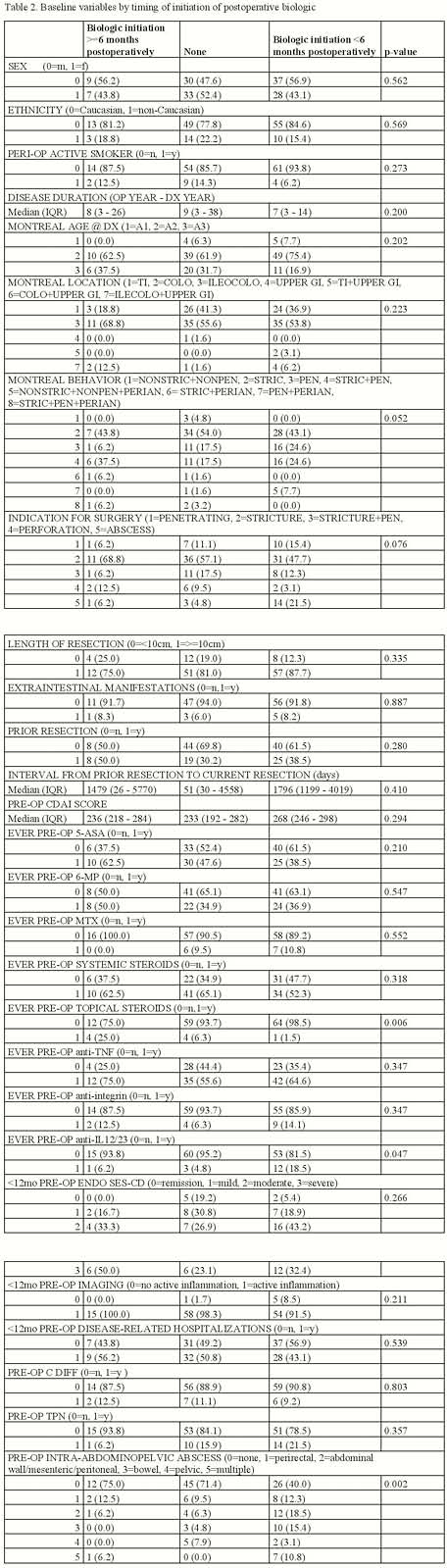
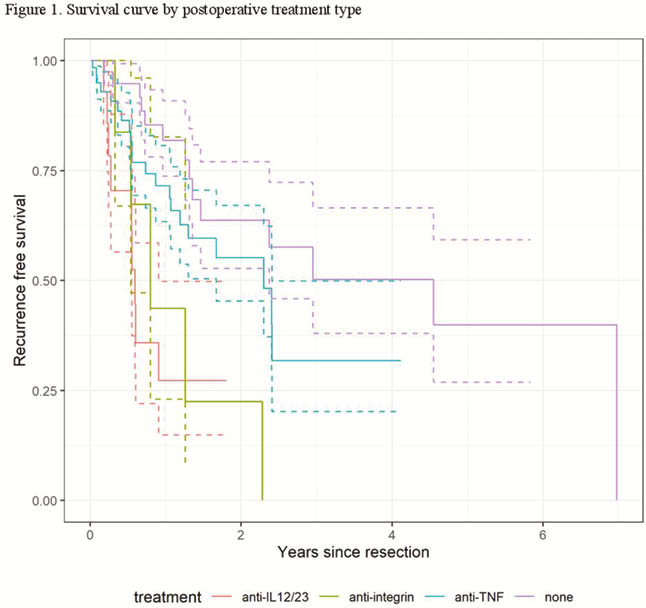
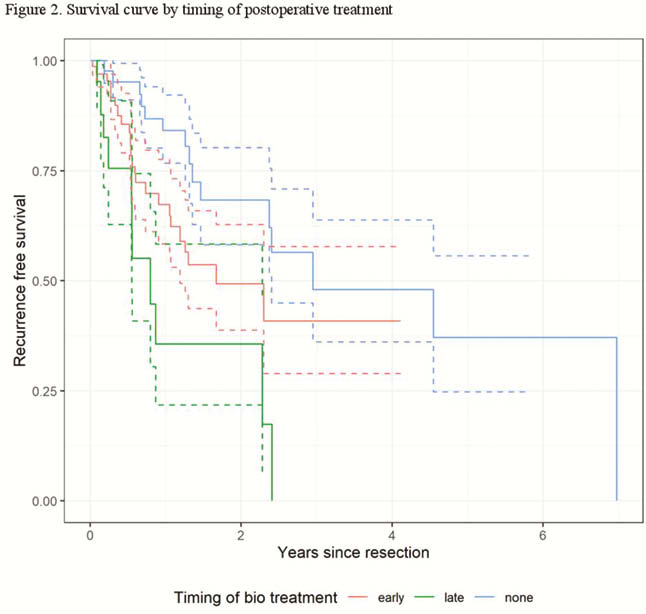
We performed a retrospective chart review of CD patients who underwent intestinal resection from 2009 to 2019 at two academic medical centres. We tabulated baseline variables against treatment groups based on the type of postoperative biologic (anti-TNF, anti-integrin, anti-IL-12/23) and timing of postoperative biologic initiation (before or after 6 months post-op). Propensity score matching was utilised for treatment groups using baseline variables as predictors. Recurrence was defined by endoscopy (>i2 Rutgeerts’ score) or radiography (active inflammation in neoterminal ileum). Survival analysis was performed to assess risk of recurrence by treatment group and timing of biologic initiation.
Results
One hundred and forty-four patients were included (51% male, 13.2% active smokers, 97.9% stricturing and/or penetrating CD, 41.7% prior resection). The majority of patients received anti-TNF therapy. Adjusting for the propensity scores, fewer patients relapsed under anti-TNF compared with anti-integrin (HR 2.87, 1.04–7.99;
Conclusion
Among propensity score-adjusted CD patients, initiation of biologics within 6 months and anti-TNF agents were superior in preventing postoperative recurrence among patients receiving postoperative biologic therapy.


