P514 Serum levels of Klotho in inflammatory bowel disease: an exploratory study
Hernandez-Camba, A.(1,2);Rodriguez-Jimenez, J.(1)*;Carrillo Palau, M.(3);Ramos Lopez, L.(3);Perez-Mendez , L.(4,5);Martin-Nuñez , E.(6);Alonso, I.(3);Vela, M.(1);Hernandez Alverez Builla, N.(3);Arranz, L.(1);Hernandez, A.(3);Ferraz Amaro, I.(7);Navarro‐Gonzalez, J.F.(6,8,9);
(1)Hospital Universitario Nuestra Señora de Candelaria, Gastroenterology, Santa Cruz de Tenerife, Spain;(2)Nursing School Nuestra Señora de Candelaria- La Laguna University, Anatomy and Histology, Santa Cruz de Tenerife, Spain;(3)Hospital Universitario de Canarias, Gastroenterology, La Laguna, Spain;(4)Hospital Universitario de Nuestra Señora de Candelaria y Gerencia de Atención Primaria, Clinical Epidemiology and Bioestadistics Division- Research Unit, Santa Cruz de Tenerife, Spain;(5)Center for Biomedical Research in Respiratory Diseases Network CIBER, Instituto de Salud Carlos III, Madrid, Spain;(6)Hospital Universitario Nuestra Señora de Candelaria, Research Unit, Santa Cruz de Tenerife, Spain;(7)Hospital Universitario de Canarias, Rheumatology, La Laguna, Spain;(8)La Laguna University, Institute of Biomedical Technologies, La Laguna, Spain;(9)Hospital Universitario Nuestra Señora de Candelaria, Nephrology, Santa Cruz de Tenerife, Spain;
Background
Alpha klotho (α-Klotho) is an anti-aging protein recognized as a humoral factor with anti-oxidant and anti-inflammatory effects, showing a bidirectional relationship with inflammation, a main pathophysiologic factor in atherosclerosis. A decrease in Klotho has been associated to cardiovascular disease (CVD), but no previous studies have investigated the relationship between inflammatory bowel disease (IBD), a risk factor for CVD, and Klotho levels. Therefore, we assessed if the serum levels of Klotho differ between patients with IBD and controls, and how this protein is related to the clinical and laboratory characteristics of the disease, subclinical atherosclerosis and metabolic risk factors.
Methods
Cross-sectional multicentric study that included 251 individuals: 191 IBD patients and 60 healthy controls was conducted. Serum Klotho levels were determined by commercial ELISA immunoassay (IBL International GmbH Laboratories). In the IBD patients disease activity was evaluated using CDAI for Crohn's disease, partial Mayo (pMayo) for ulcerative colitis, specific laboratory parameters, determination of the Systematic Coronary Risk Evaluation (SCORE), and the presence of subclinical atherosclerosis was assessed using carotid ultrasound for identifying carotid plaque and measurement of carotid intima-media thickness.
Results
Serum Klotho levels were significantly higher in the IBD group: 734.31 pg/ml vs. 484.17 pg/ml (p<0.001) compared with controls. In the IBD group, no significant differences in the serum Klotho levels were found between the type of IBD (p=0.911), time from diagnosis (p=0.126), disease activity: CDAI (p=0.277), pMayo (p=0.916), type of treatment (0.76), the presence of plaque (p=0.101) or the intima media thickness (p=0.429). However, a significant inverse correlation between serum Klotho and the SCORE was observed in IBD patients: r = -0.176 (p= 0.014) (figure 1)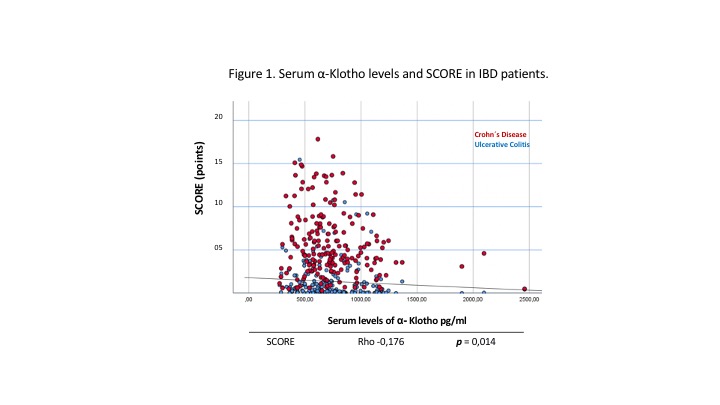
Conclusion
Patients with IBD had higher Klotho levels than healthy controls, with an inverse and significant relationship with the SCORE in the IBD patients. Further studies are necessary to clarify the role of Klotho in IBD.


