P547 Inadequate vitamin C status and association with inflammatory biomarkers in adults with active Crohn’s disease
C. Wall1, K. MacFarlane2, A. Carr3, A. Day4, R. Gearry1
1Department of Medicine, University of Otago, Christchurch, New Zealand, 2Gastroenterology Department, Christchurch Hospital, Christchurch, New Zealand, 3Department of Pathology and Biomedical Sciences, University of Otago, Christchurch, New Zealand, 4Department of Paediatrics, University of Otago, Christchurch, New Zealand
Background
Micronutrient deficiencies are common in inflammatory bowel disease (IBD) due to the inflammatory burden and changes in dietary intake. Vitamin C, an essential water-soluble antioxidant required for tissue repair and immune function, is found primarily in fresh fruit and vegetables however, this food group is more often avoided by people with IBD compared with the general population. This research aimed to determine serum vitamin C status in subjects with active Crohn’s disease, measure urinary vitamin C excretion in healthy controls (HC) and Crohn’s disease patients before and after exclusive enteral nutrition (EEN) and assess associations between inflammatory markers and vitamin C.
Methods
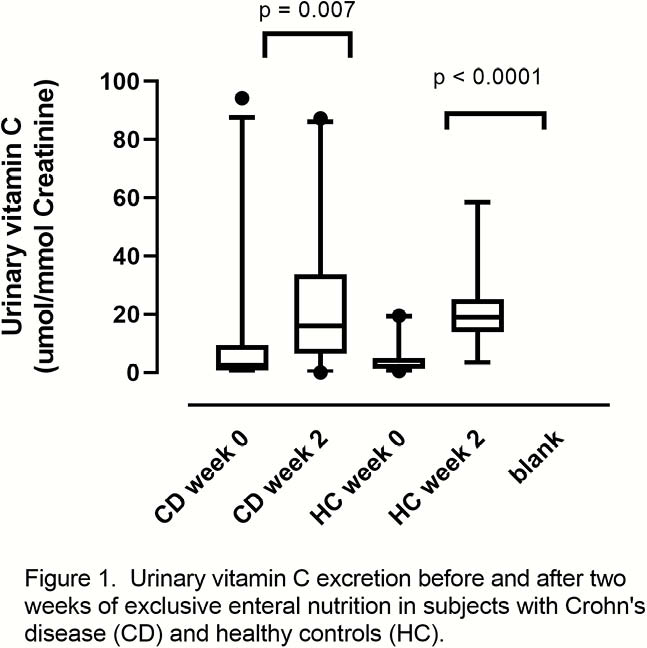
Stored serum and random urine samples prospectively collected from adults with mild to moderately active Crohn’s disease and adult HC were analysed. Both HC and Crohn’s disease groups received EEN with a known vitamin C content for two weeks. Serum and urinary vitamin C were measured using high-performance liquid chromatography with electrochemical detection. Urinary vitamin C was standardised to urinary creatinine. Non-parametric t-tests and correlations were performed.
Results
EEN was initiated in 38 patients (aged 16 to 39 years old). Inadequate serum vitamin C (<50 µmol/l) was present in 36/38 patients with active Crohn’s disease and 45% had hypovitaminosis C. Baseline C-reactive protein (CRP) was 12 mg/l (range, 3 to 158 mg/l) and faecal calprotectin was 1065 µg/g (range, 60 to 3838 µg/g). Serum vitamin C correlated weakly with CRP (
Conclusion
Patients with active Crohn’s disease had inadequate vitamin C status. EEN increased urinary vitamin C excretion in both Crohn’s disease and HC, suggesting low baseline dietary vitamin C intake and potentially enhanced utilisation. Further research with a larger patient cohort would provide a greater understanding of vitamin C metabolism in active Crohn’s disease.


