P547 Rate of Colectomy Increases within Twelve Months of Sequential Therapy for Ulcerative Colitis
Barnes, E.(1)*;Zhang, X.(2);Long, M.(3);Herfarth, H.(1);Kappelman, M.(4);
(1)University of North Carolina at Chapel Hill, Division of Gastroenterology and Hepatology, Chapel Hill, United States;(2)University of North Carolina School of Medicine, Center for Gastrointestinal Biology and Disease, Chapel Hill, United States;(3)University of North Carolina at Chapel Hill, Division of Gastroenterology & Hepatology, Chapel Hill, United States;(4)University of North Carolina at Chapel Hill, Division of Pediatric Gastroenterology, Chapel Hill, United States;
Background
Even the best medical treatments for ulcerative colitis (UC) are often ineffective, with up to 15% of patients requiring a colectomy within the first 10 years of diagnosis. In the current era, patients have access to an increasing number of medical therapies that may prevent and/or delay surgery. To evaluate the relative effectiveness of sequential therapies for UC, we evaluated the 12-month colectomy rate among patients switching to a second, third, or fourth-line biologic or small molecule therapy for UC.
Methods
We conducted a retrospective cohort study, using a new-user design, evaluating patients with commercial insurance in the MarketScan database between 2000 and 2019. The index date for the study was defined as the date of the first claim for a second, third, or fourth biologic or small molecule therapy. The primary outcome was defined as colectomy-free survival at 12 months after the index date. Significance of 12-month colectomy rates over time was evaluated using the Cochran-Armitage test of trend and a Generalized Estimating Equation (GEE) model adjusting for age (18-35, 36-55, >55), sex and index year (year 2007-2014 and 2015-2019).
Results
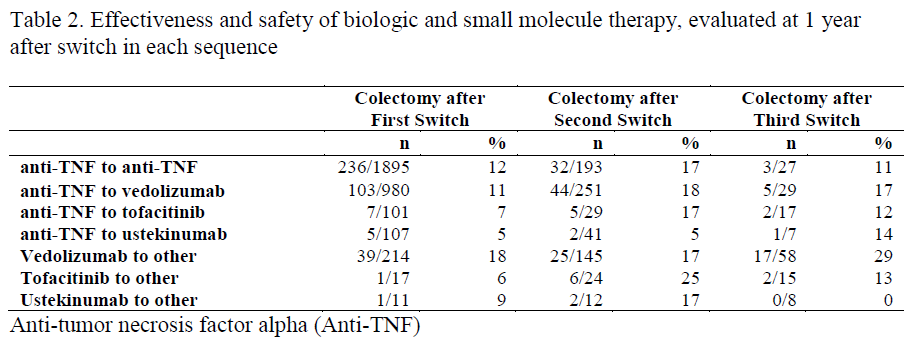
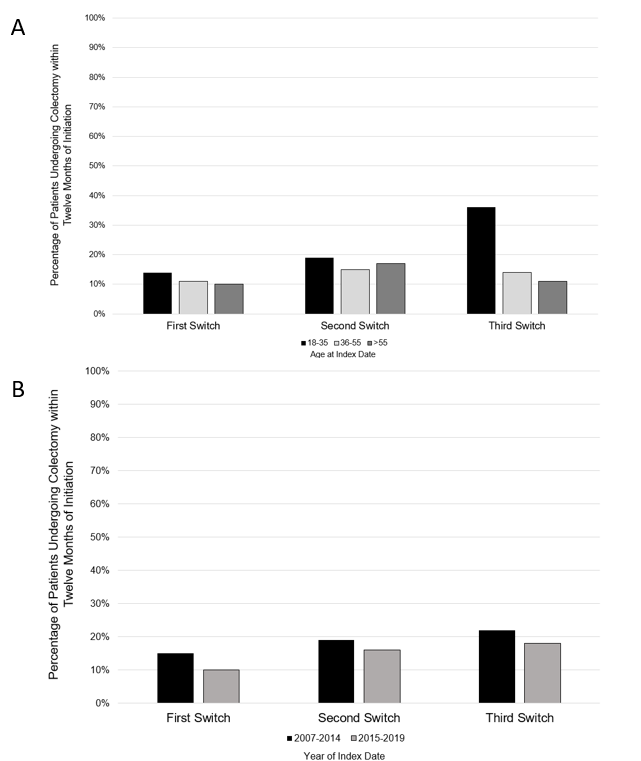
We identified 3,325 patients with UC that made at least 1 switch in biologic or small molecule therapy during the study period. Among these, 50% were female and the median age was 41 years (interquartile range 31-52 years, Table 1). The most frequent initial biologic switches were from an anti-tumor necrosis factor alpha (TNF) to an anti-TNF (1895 patients [57%]) and anti-TNF to vedolizumab (980 patients [30%]) were the most common sequences of therapies (Table 2). Overall, 392 (12%) patients underwent colectomy within 12 months of the first switch while 116 of 695 (17%) patients underwent colectomy within 12 months of the second switch. Among 161 patients that underwent 3 switches, 30 (19%) underwent colectomy within 12 months of the third switch (p<0.001, Table 3). The rate of UC-related hospitalizations in the 12 months after switch also increased significantly with each subsequent switch (11% vs. 15% vs. 19% for first, second and third switches respectively, p<0.001). The colectomy rate per switch in therapy appeared stable when stratifying by index date and age at index date (Figure 1).

Conclusion
Despite increases in the number of available mechanisms for the treatment of UC, a substantial proportion of patients will still require colectomy for UC. The absolute risk of colectomy within 12 months and other negative outcomes increase with each subsequent treatment. These data can help inform complex decisions regarding the timing of surgery relative to initiation of subsequent therapy in patients with medically-refractory disease.


