P555 Systematic review with meta-analysis: The impact of cancer treatments on the disease activity of inflammatory bowel diseases
Grimsdottir, S.(1);Attauabi, M.(1,2)*;Dahl, E.K.(1);Burisch, J.(2,3);Seidelin, J.B.(1);
(1)Copenhagen University Hospital - Herlev and Gentofte- Herlev, Department of Gastroenterology and Hepatology, Herlev, Denmark;(2)University of Copenhagen- Hvidovre Hospital, Copenhagen Center for Inflammatory Bowel Disease in Children- Adolescents and Adults, Hvidovre, Denmark;(3)Copenhagen University Hospital - Amager and Hvidovre- Hvidovre, Gastrounit- Medical Division, Hvidovre, Denmark;
Background
The association between cancer treatments and exacerbation of IBD is unclear. We aimed to evaluate the effects of cancer treatments on the disease activity of IBD.
Methods
We performed a systematic review of the literature on cancer therapy in patients with pre-existing IBD. Electronic searches of PubMed, Cochrane Library, and Embase were combined with manual searches (September 2021). Meta-analysis was performed using the random-effects model. The primary outcome was flares of IBD following cancer therapy. Secondary outcomes were need for IBD-related hospitalization, surgery, and initiation or intensification of steroid or biological treatments to manage IBD flares.
Results
In total, 33 studies were included in the systematic review, comprising 1,298 patients with IBD who received cancer treatment (Figure 1). The overall occurrence of IBD flares following cancer treatment was 30% (95% confidence interval (CI) 23-37%, Figure 2). IBD flares resulted in utilization of systemic steroids and biologic therapies among 25% and 10%, respectively, and in discontinuation of cancer treatment among 8% of patients (Figures 3a and 3b). Finally, risk of gastrointestinal toxicity following immune check point inhibitor treatment (ICI) was increased in patients with IBD compared to patients without IBD (RR=3.62, 95% CI 2.89-4.78) (Figure 4). Despite this, the studies generally reported that flares were manageable. 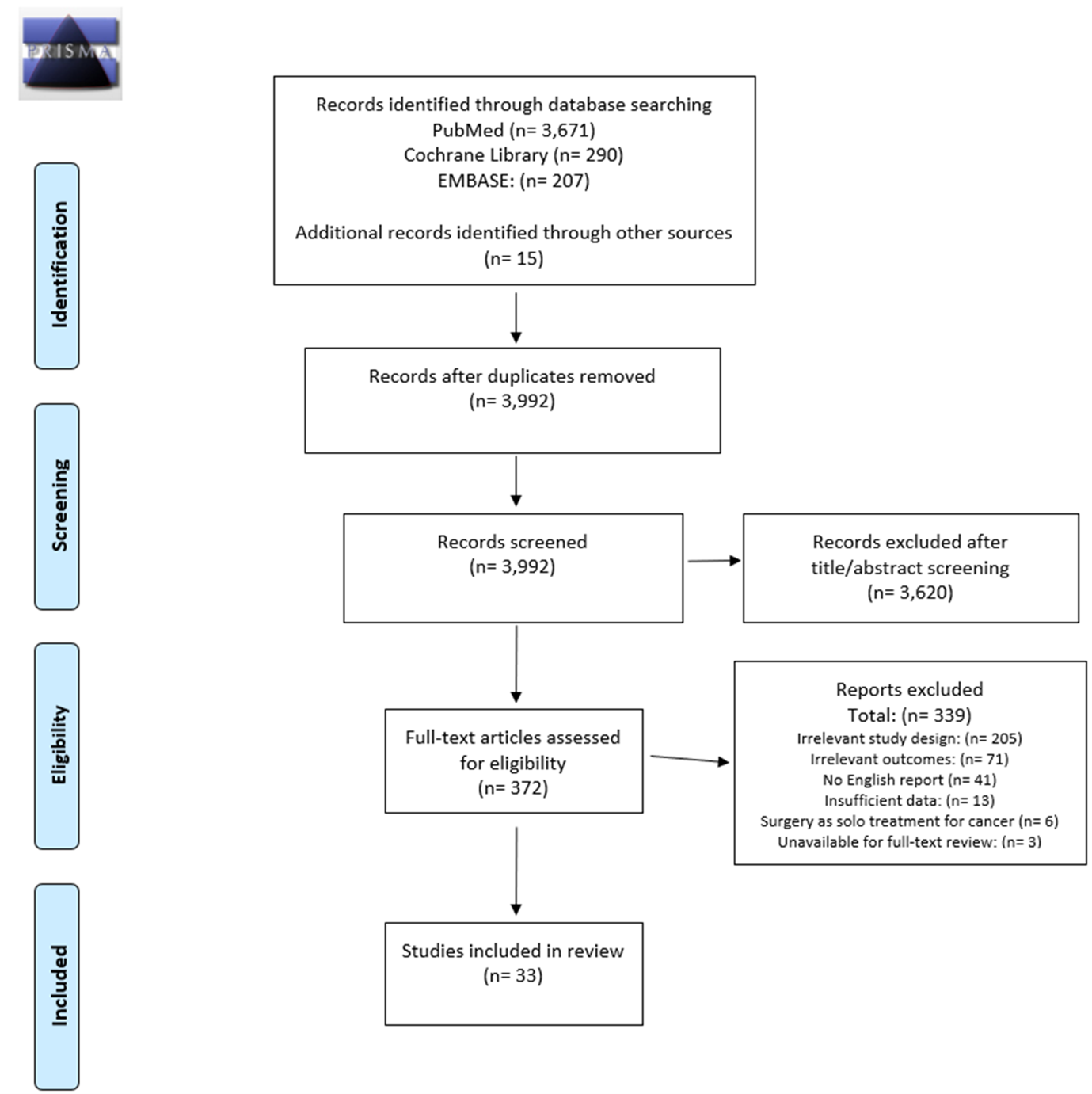
FIGURE 1. Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) flow diagram summarizing study selection.
FIGURE 2: Forest plot of incidence of IBD flares following cancer therapy, grouped by cancer treatment.
FIGURE 3: Forest plot of incidence of need for initiation of a) systemic steroids or b) initiation or intensification of biologic therapyfor managing IBD flares following cancer treatment.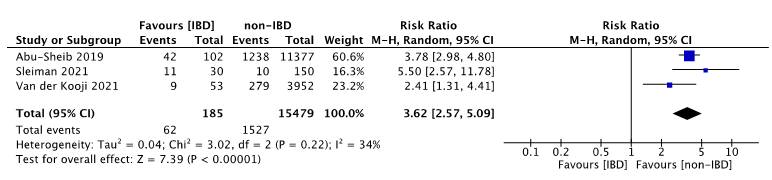
FIGURE 4: Forest plot of risk ratios of GI toxicities following cancer treamtment in patients with IBD vs patients without IBD.
Conclusion
Current data indicate a high proportion of patients with IBD experiencing a flare following the start of cancer treatment. Patients with IBD were at increased risk of gastrointestinal toxicity following ICI treatment compared to those without IBD. However, cancer therapy-induced IBD flares were manageable and should not preclude appropriate cancer treatments.


