P561 The management of Crohn’s disease (CD) patients post ileocaecal resection: a multicentre, regional audit in Northern England
S. BATCHELOR1, A. Speight2, Gastroenterology Research and Audit for Northern Trainees
1Department of Gastroenterology, Freeman Hospital, Newcastle upon Tyne, UK, 2Department of Gastroenterology, Royal Victoria Infirmary, Newcastle upon Tyne, UK
Background
70% of patients with Crohn’s disease (CD) require intestinal resection.1 Post-operative recurrence (POR) is common with 70% of patients requiring further surgery in the pre-biologic era.2 ECCO guidelines suggest identifying patients at risk of recurrence (disease phenotype, smoking, prior resection), the use of imidazole antibiotics following surgery and assessment for recurrence within 12 months. The ECCO guidelines recommend ileocolonoscopy, although alternative modalities can be used. The Rutgeerts score predicts POR and is recommended to establish the need for preventative treatment.3 The aim of this study was to undertake a region-wide audit of practice with regards to post-operative CD in the Northern region.
Methods
A regional, multicentre, retrospective audit was conducted by GRANT, a network of gastroenterology trainees in Northern England. Data collection was performed for CD patients who had an ileocaecal resection between 1/9/16 and 1/9/17. Patients with an end-ileostomy were excluded. Patients were identified using clinical coding and data collection sheets were completed.
Results
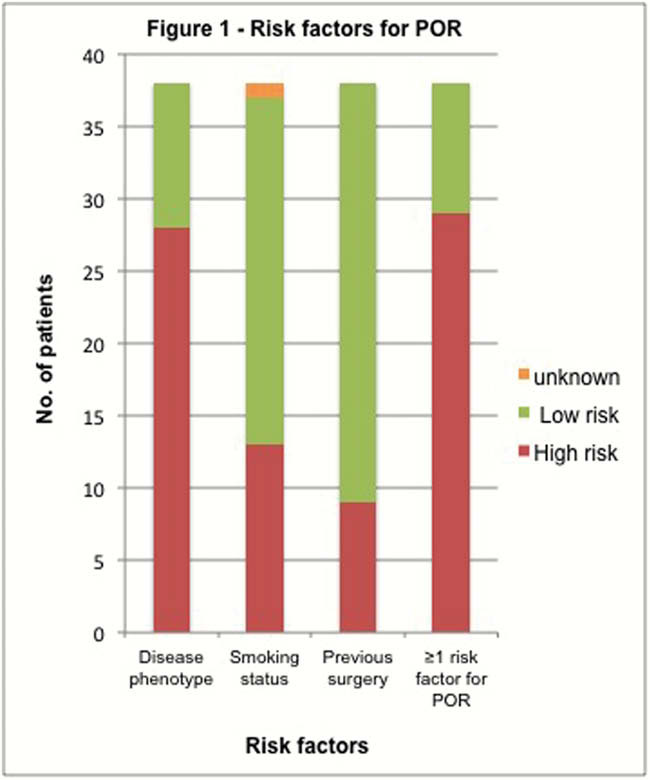
Seven of 9 Hospital Trusts returned data. The number of eligible patients was 38 with a mean age of 41 years. Seventy-six per cent (29/38) patients had at least one risk factor rendering them ‘high-risk’ for POR (Figure 1). Only 13% (5/38) of patients received imidazole antibiotics postoperatively and only 29% (11/38) had an ileocolonoscopy within 12 months. However, 32% (12/38) had an alternative assessment of POR, with calprotectin being the most popular. An escalation in treatment following assessment was required in 25% (9/38) of patients. Postoperatively, 40% (15/38) of patients had no maintenance therapy before POR assessment; 26% (10/38) continued on the same therapy as preoperatively and34% (13/38) had augmented pre-operative therapy.
Conclusion
The majority of patients in Northern England who have an ileocaecal resection for CD are high risk for recurrence and many patients are not being assessed. Endoscopic POR predates clinical POR [4] and, without monitoring, the opportunity to augment therapy and prevent clinical recurrence can be missed. In Northern England, less invasive disease monitoring is being used to assess for POR and this audit would suggest that these have a comparable rate of identifying a need to escalate maintenance therapy. A postoperative CD management bundle is being developed and will be implemented to assess whether this drives improvement.


