P580 Early intestinal ultrasound assessment predicts endoscopic response and remission on anti-TNF treatment in Crohn’s Disease – a prospective longitudinal cohort study
de Voogd, F.(1);Bots, S.(1);Gecse, K.(1);Gilja, O.H.(2);D'Haens, G.(1);Nylund, K.(2);
(1)Amsterdam University Medical Center, Gastroenterology and Hepatology, Amsterdam, The Netherlands;(2)Haukeland University Hospital, National Centre for Ultrasound in Gastroenterology, Bergen, Norway;
Background
In the assessment of treatment response in Crohn’s Disease (CD) objective measures are superior to clinical improvement. Intestinal ultrasound (IUS) is an emerging modality with high accuracy to detect CD disease activity. Less is known about early transmural changes at IUS in treatment follow-up. Therefore, we aimed to investigate conventional IUS and contrast-enhanced ultrasound (CEUS) parameters and how they are associated with endoscopic treatment response.
Methods
In this longitudinal prospective cohort study, consecutive patients with active CD according to the simplified endoscopic score (SES-CD≥3) starting anti-TNF-α treatment were included. We recorded clinical, biochemical, IUS and CEUS parameters at baseline (T0), after 4-8 weeks (T1) and at 12-34 weeks (T2). IUS parameters were scored as previously established1. The SES-CD was scored per segment by a gastroenterologist immediately after endoscopy. The bowel segment with highest SES-CD score and thickest wall on IUS was identified. At T2, endoscopic response (decrease SES-CD≥50%) and endoscopic remission (SES-CD=0) were scored per segment. IUS and CEUS were scored blindly by two readers using recorded videos.
Results
40 patients were included (Table 1) with 23 completing follow-up. The other 17 patients had side-effects and stopped treatment (n=9), underwent bowel surgery (n=5) or were lost to follow-up (n=3). At T2, 14 reached endoscopic remission, 17 had endoscopic response. The absolute decrease in BWT at T1 and T2 paralleled endoscopic response (Figure 1). Decrease in BWT of 18% at T1 (Fig 2) predicted endoscopic response accurately (OR: 10.8, 95%CI: 1.7-69.0, p=0.012). For T2, 29% decrease in BWT (Fig 2) was most accurate to determine endoscopic response (OR: 37.5, 95%CI: 2.8-507.5, p=0.006). At T2, a BWT of 3.2 mm was most accurate (AUROC: 0.940, 95%CI: 0.862-1.000, p<0.0001, sensitivity: 92%, specificity: 85%) to determine endoscopic remission (OR: 39.4, 95%CI: 7.7-202.6, p<0.0001). Normalization of Colour Doppler Signal (CDS) (no signal or single vessel) (OR: 13.8, 95%CI: 1.3-147.8, p=0.03) or Wash-out Rate (WoR) at CEUS (1 dB increase: OR: 0.8, 95%CI: 0.60-0.96, p=0.019) added significantly to BWT to determine endoscopic remission at T2.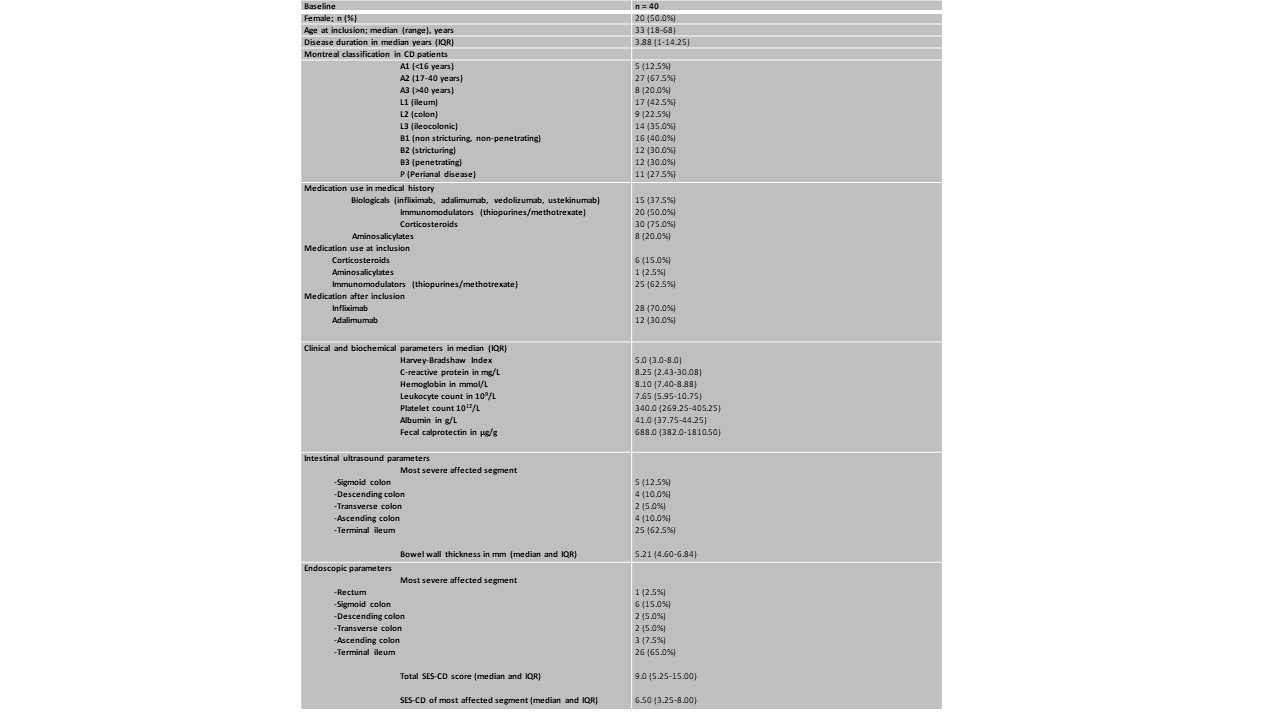
Table 1: Baseline characteristics 
Figure 1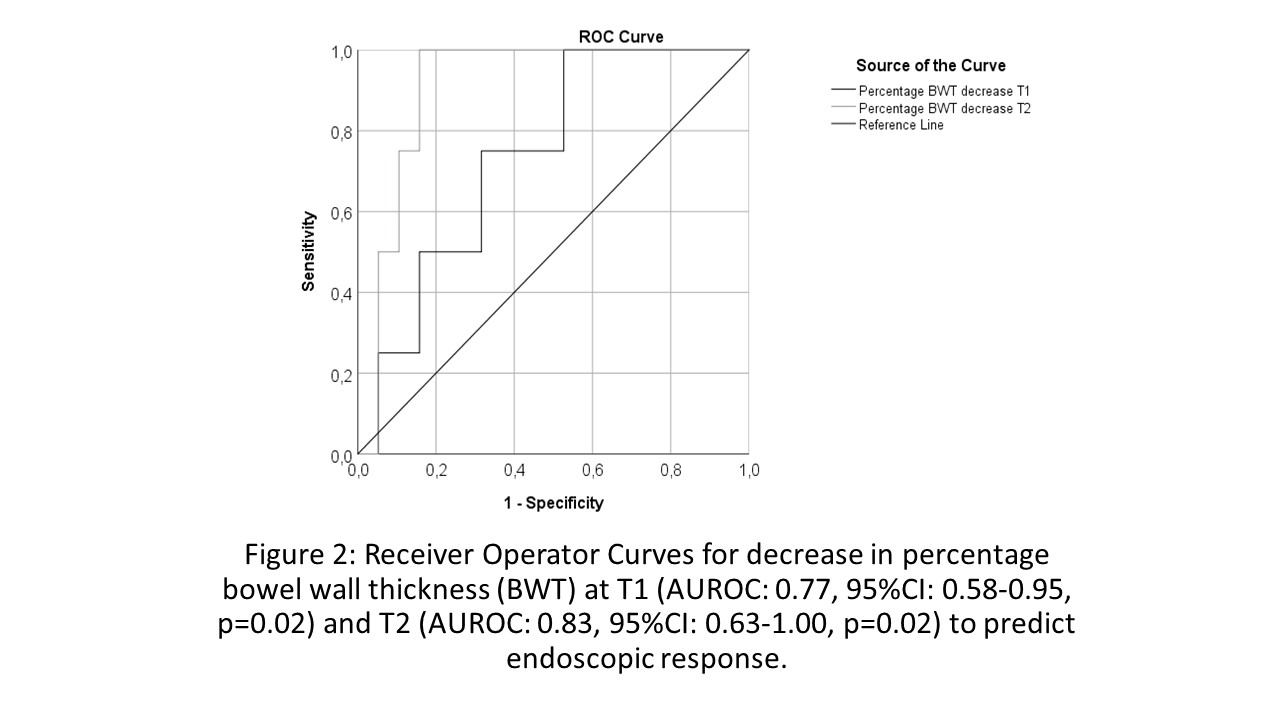
Figure 2
Conclusion
Decrease of BWT 4-8 weeks after treatment initiation predicted endoscopic response later during follow-up. In addition, we have provided accurate cut-off values for (Δ)BWT associated with endoscopic response and remission at different time-points. CDS or WoR were both of additional value to determine endoscopic remission after 12-34 weeks. As CEUS is time consuming, CDS might be sufficient in the close follow-up of CD patients.
1. Novak et al, JCC 2021


