P651 Comparison of Adverse Events of SARS-CoV-2 Vaccination between Patients with Inflammatory Bowel Disease and Healthcare Workers
Kim, J.(1)*;Sagong, M.(1);Lee, Y.J.(1);Kim, K.O.(2);Kim, E.S.(3);Kim, E.Y.(4);Jang, B.I.(2);
(1)Keimyung University School of Medicine, Department of Internal Medicine, Daegu, Korea- Republic Of;(2)Yeungnam University College of Medicine, Department of Internal Medicine, Daegu, Korea- Republic Of;(3)Kyungpook National University School of Medicine, Department of Internal Medicine, Daegu, Korea- Republic Of;(4)Daegu Catholic University of School of Medicine, Department of Internal Medicine, Daegu, Korea- Republic Of;
Background
This study aimed to investigate the adverse events (AEs) after SARS-CoV-2 vaccination in patients with inflammatory bowel disease (IBD) and to compare them with healthcare workers (HCWs).
Methods
We conducted a web-based survey on the local and systemic AEs experienced within 7 days of SARS-CoV-2 vaccination (BNT162b2, mRNA-1273, or ChAdOx1 nCoV-19) in IBD patients and HCWs between October 2021 and February 2022. The frequency of all AEs was compared between IBD patients and HCWs, and propensity score matching method was used to control confounding factors.
Results
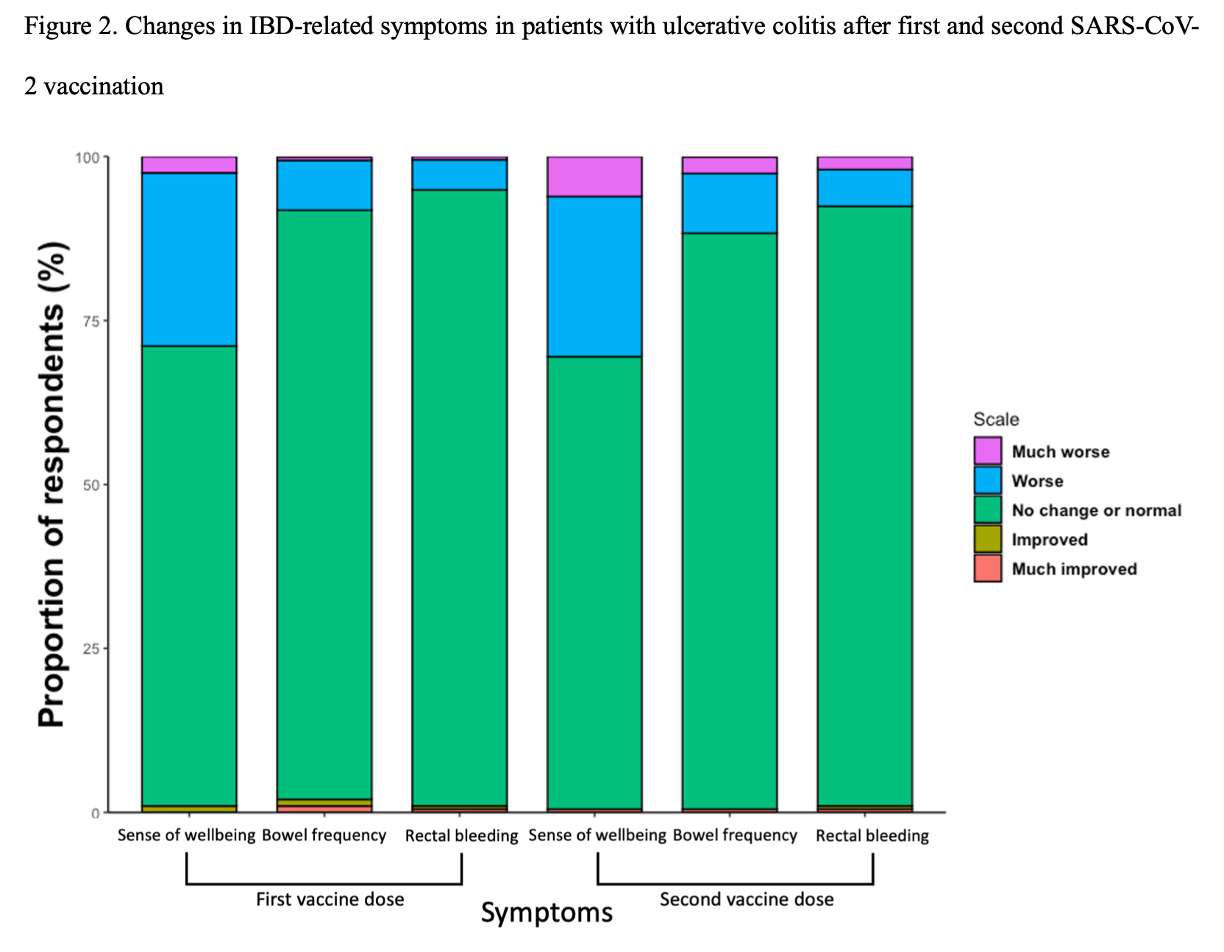
A total of 336 IBD patients (139 Crohn’s disease [CD] and 197 ulcerative colitis [UC]) and 288 HCWs who completed the questionnaire had received the same type of vaccine for their first and second doses. Common local AEs in patients with IBD were injection site pain (78.9% and 70.8% after receiving first and second vaccine doses, respectively), swelling (35.4% and 31.5%), and induration (35.1% and 26.5%), and systemic AEs were fatigue (44.6% and 42.0%), myalgia (42.6% and 37.2%), and fever or febrile sense (29.5% and 32.1%). All severe AEs were rarely observed (0-3.9%). Hospital visits or hospitalizations associated with AEs were observed in 16 (4.8%) and 18 (5.4%) patients, respectively. A small number of patients reported deterioration of bowel frequency (CD: 10.1% and 12.2%, UC: 8.1% and 11.7%), abdominal pain (CD: 5.0% and 7.9%), and rectal bleeding (UC: 5.1% and 7.6%). About 30% of IBD patients reported a worsening of their sense of well-being. After propensity score matching, there was no significant increase in the frequency of AEs in IBD patients except for diarrhea (14.5% vs 4.8%, P = 0.005) and dyspepsia (15.2% vs 5.5%, P= 0.007) after first vaccination.
Conclusion
SARS-CoV-2 vaccination in patients with IBD was generally well-tolerated and severe AEs occurred rarely. Compared with HCWs, the frequency of AEs does not seem to increase except for diarrhea and dyspepsia.