P670 “What Matters To You?” – How do patient views compare with a patient experience framework and UK national standards of care?
Sheldon, E.(1)*;Roman, S.(2);Randall, K.(2);Rachel, H.(3);Winsor, G.(4);Wakeman, R.(5);Lobo, A.(2);
(1)The University of Sheffield, School of Health and Related Research, Sheffield, British Virgin Islands;(2)Sheffield Teaching Hospitals NHS Foundation Trust, Gastroenterology, Sheffield, United Kingdom;(3)The University of Sheffield, School of Health and Related Research, Sheffield, United Kingdom;(4)Crohn's & Colitis UK, Research & Quality Improvement, Hatfield, United Kingdom;(5)Crohn's & Colitis UK, Services- Advocacy & Evidence, Hatfield, United Kingdom; on behalf of the AWARE-IBD Study Group
Background
There is increasing focus on the organisation of services for people with IBD. Patient experience of care is an important consideration in service delivery. The United Kingdom NHS Long Term Plan indicates the importance of support that is more differentiated for individuals, with more personalised care when needed, which starts with the question ‘What matters to you?”. This is particularly important for people with inflammatory bowel disease (IBD).
Methods
The aim was to identify ‘What matters to you?’ for people attending a single UK teaching centre IBD service and to relate it to patient experience and national standards of care. Invitations to take part in the AWARE-IBD quality improvement programme were sent to 4082 patients receiving IBD care at a single UK teaching centre in 2 rounds (October 2021 and May 2022). Invitation letters included an anonymous open-ended questionnaire asking patients “what matters to you?”. Responses were extracted as qualitative data and coded using two frameworks: Patient experience domains (Bull et al) (Communication, Patient-centred Care, Quality, Integration, Involvement, Accessibility, Environment and Facilities, Discomfort) and national IBD UK Standards. Frequencies for each coding strategy were calculated to determine the most important patient experience domains and IBD UK standards.
Results
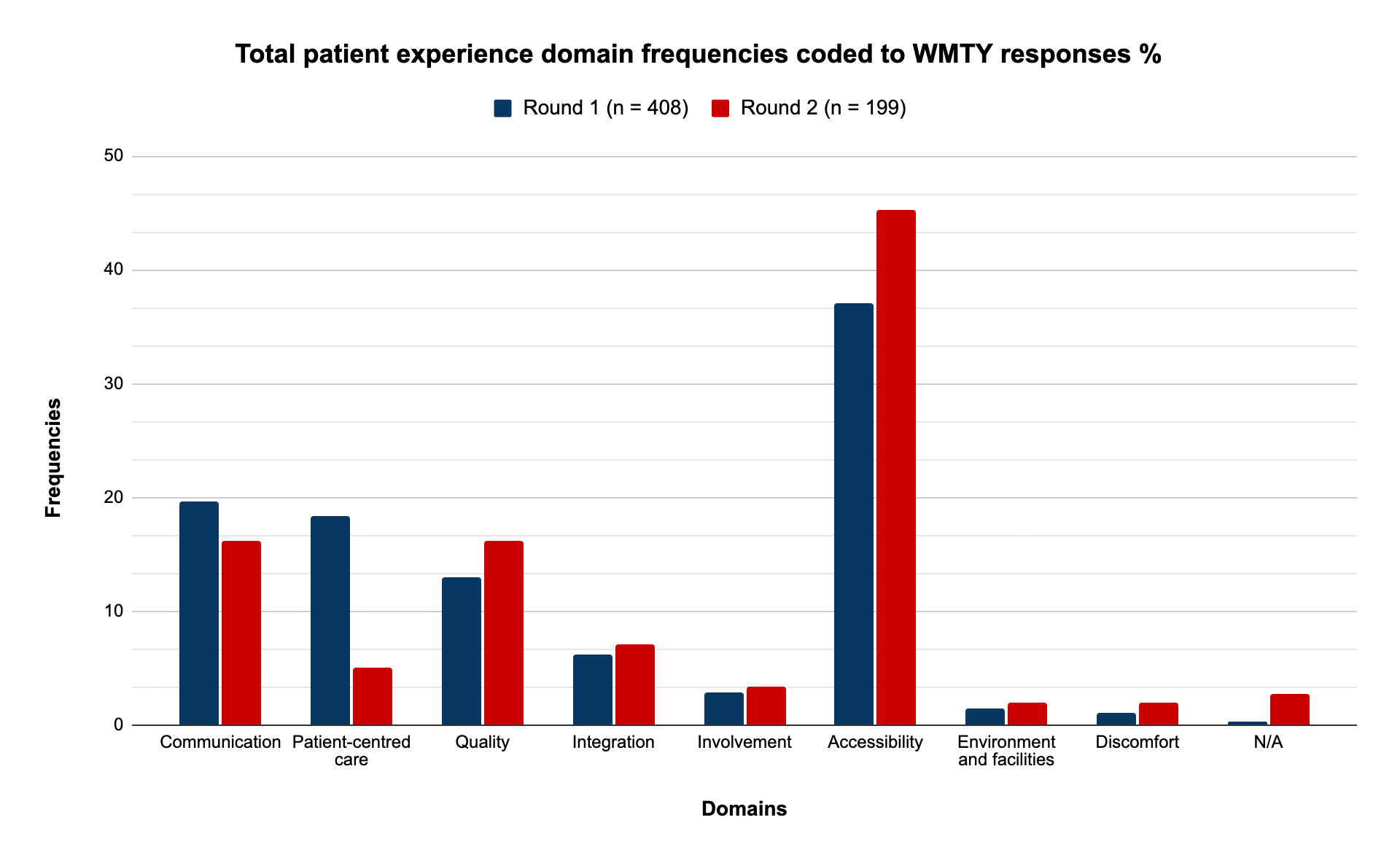
Responses were received from 408 and 205 patients from each recruitment round (n=613). Figure 1 displays frequencies for each patient experience domain. Accessibility (47.5% and 53.2% respectively), Communication (19.6% and 12.7%) and Patient-Centred Care (15.7% and 11.2%) were expressed most frequently. Sub-themes included access to and contact with IBD nurse specialists, timely and accessible appointments and regular contact with a specialist IBD health care professional (HCP). Responses were coded to IBD UK standards, where possible (Table 1). Responses most frequently coded to statements relating to shared decision making, having a personalised care plan, access to an IBD nurse specialist including helpline and regular clinical review. 77 responses could not be coded to an IBD UK standard.

Conclusion
Access to the IBD service when needed matters most to patients with good communication of information and personalised, patient-centred care. Service organisation should therefore reflect these facets of patient experience and defined standards. Patient views that are not currently represented in published standards should be considered in future iterations. This study also highlights personalised written care plans and improved access to the IBD Nurse Advice line.


