P778 Longitudinal trajectory of fatigue in inflammatory bowel disease patients: a prospective study
N. Borren1, M. Long2, J. van der Woude3, R. Sandler2, A. Ananthakrishnan1
1Massachusetts General Hospital, Division of Gastroenterology, Boston, USA, 2University of North Carolina, Gastroenterology, Chapel Hill, USA, 3Erasmus University Medical Center, Gastroenterology & Hepatology, Rotterdam, The Netherlands
Background
Fatigue is a commonly reported and sometimes disabling symptom in patients with inflammatory bowel disease (IBD). Its prevalence, mechanism, and impact remain poorly understood. Using a large cohort of patients with IBD, we aimed to prospectively determine the trajectory of fatigue and to identify determinants and impact of incident and prevalent fatigue on patients with IBD.
Methods
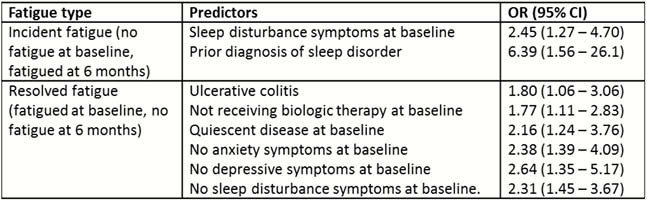
This prospective study was nested within the IBD partners cohort, a validated internet-based cohort of patients with IBD. Participants were invited to prospectively complete questionnaires assessing fatigue status at baseline and subsequently after 6 and 12 months. Fatigue was assessed using the validated Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F) score. A FACIT-F score of < 43 was defined as significant fatigue. We examined the trajectory and predictors of different courses of fatigue including incident fatigue (not fatigued as baseline but fatigued at 6 months) and resolved fatigue (fatigue at baseline but resolved on follow-up).
Results
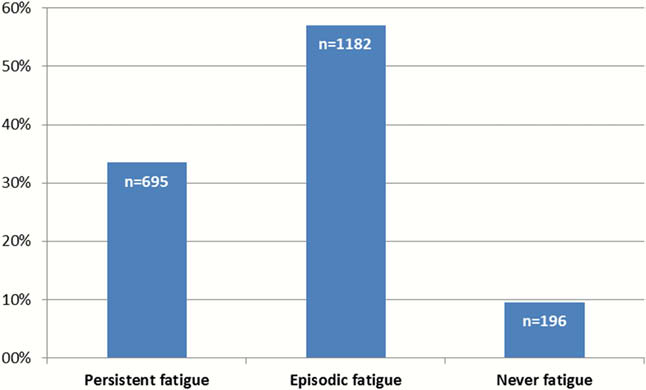
A total of 2429 patients (1605 CD, 824 UC) completed baseline assessment among whom 1057 completed a second assessment at 6 months. First, we identified three distinct patterns of fatigue. Episodic fatigue defined as fatigue at any one (but not both) time point was the most common, affecting 1182 patients (57.0%). Persistent fatigue (at both baseline and follow-up) affected 33.5% (
 |
Conclusion
Our findings indicate three distinct trajectories of fatigue in patients with IBD with their distinct predictors. Importantly, 26% of patients developed new onset fatigue at 6 months demonstrating the substantial impact of this on patients with IBD.


