P802 Relationships between validated clinical, endoscopic and histological indices in ulcerative colitis
Walsh, A.(1);Kormilitzin, A.(1);Friedrich, M.(1);Pakpoor, J.(1);HosackMBChB MSc MRCP, T.(1)*;Matini, L.(1);Kantschuster, R.(1);Sharda, A.(1);Dunbar, G.(1);Cheung, V.T.F.(1);Ambrose, T.(1);Brain, A.O.(1);Palmer, R.(1);Satsangi, J.(1);Travis, S.P.L.(1);
(1)University of Oxford, Translational Gastroenterology Unit- Biomedical Research Centre- Mathematical Institute and Kennedy Institute, Oxford, United Kingdom;
Background
The simple clinical colitis activity index (SCCAI) is increasingly used in practice for monitoring symptoms, because it documents urgency and nocturnal stool frequency, which are excluded from other indices. The question is how the SCCAI relates to validated endoscopic and histological indices, so that SCCAI thresholds for remission and active disease can be defined.
Methods
The SCCAI (range 0-19) was collected in real time from patients with ulcerative colitis (UC) using web-based TrueColours-IBD monitoring and collated with endoscopic activity (UCEIS, 0-8) and Nancy histological index (NHI, 0-4) for patients who had recorded SCCAI data up to 14d before endoscopy.
Results
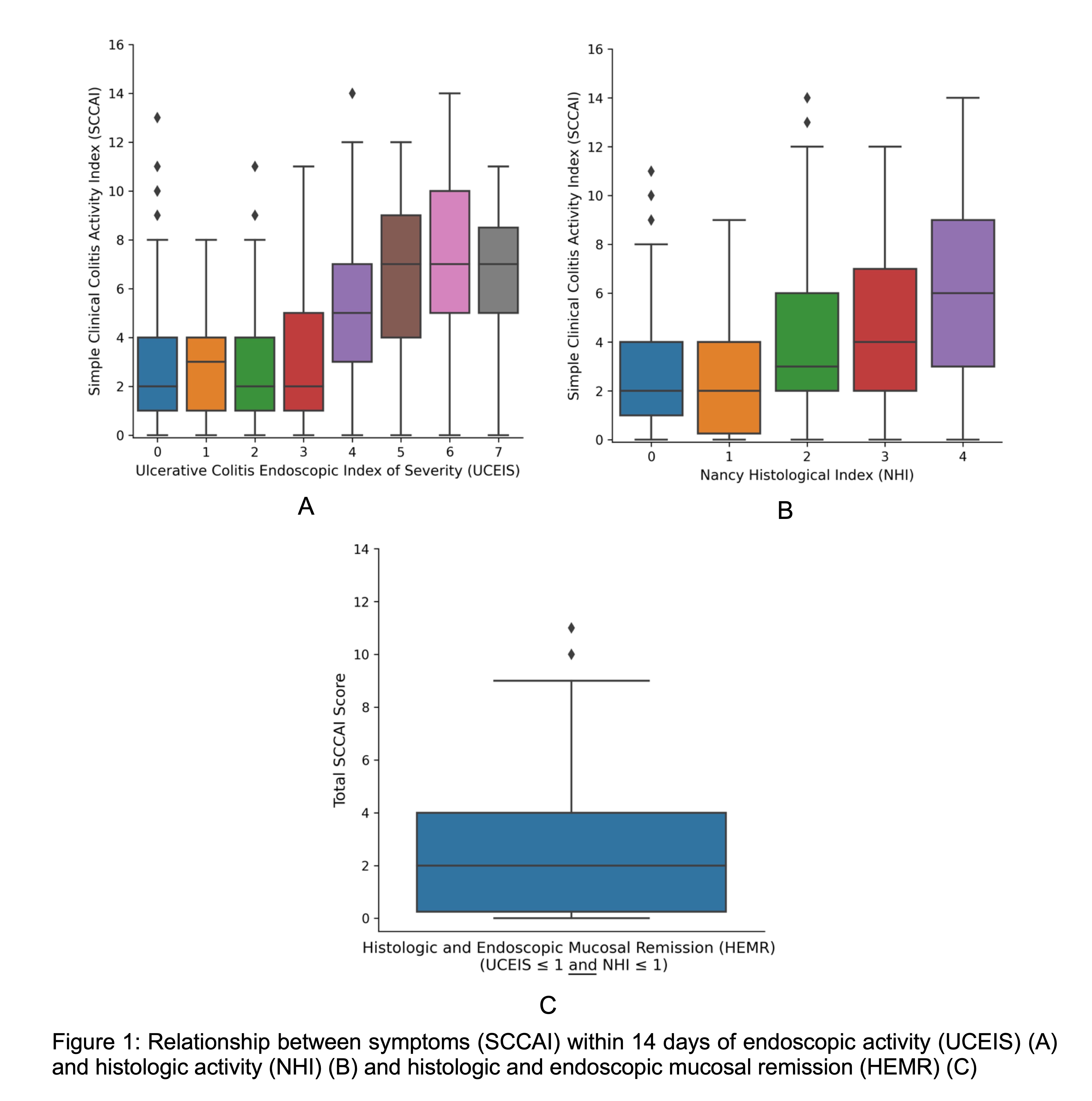
482 SCCAI/endoscopy/biopsy trios were analysed from 323 unique patients (162 male) aged 18 to 86 years (male: mean = 43.8, SD = 15.9; female: mean = 44, SD = 14.9). Disease extent for male: Normal=48, E1=23, E2=116, E3=43, female: Normal=45, E1=42, E2=110, E3=27. Spearman's rank correlation coefficient between UCEIS and NHI scores was r=0.77 (95% confidence interval [CI] 0.72 - 0.82, p <0.001). When the UCEIS was ≤ 1, or NHI ≤ 1, which is consistent with remission, the median (IQR) SCCAI was 2 (1 to 4) (Fig 1A, 1B). When the SCCAI was ≥5, the median (IQR) UCEIS was 4 (3 to 5) and the median (IQR) NHI was 3 (2 to 4). For patients with both histologic and endoscopic mucosal remission (HEMR), defined as NHI ≤ 1 and UCEIS ≤ 1, the median (IQR) SCCAI was 2 (0.25 to 4) (Fig 1C). Patients with SCCAI scores outside the IQR (n=8 for UCEIS, n=5 for NHI) had symptoms primarily driven by bowel urgency or poor general wellbeing. Four groups of patients could be identified using linear regression analysis modelling of relationships between bowel urgency and UCEIS score: ‘no urgency without active disease’; ‘urgency without active disease’; ‘urgency with active disease’; and ‘no urgency with active disease’ (Fig 2).

Conclusion
There is a ‘grey zone’ at low scores of symptom-based indices that cannot discriminate endoscopic or histologic remission from mildly active disease. The SCCAI threshold for active UC is >5, but with wide confidence intervals. Mechanisms behind symptoms in the absence of active inflammation need investigating.


