P809 The impact of different treatment strategies in newly diagnosed patients with Crohn’s Disease: a multicentre study
Revés, J.(1)*;Morão, B.(1);Montanaro, G.(2);Sciberras, N.(2);Bravo, A.C.(1);Glória, L.(1);Ellul, P.(2);Torres, J.(1);
(1)Hospital Beatriz Ângelo, Gastroenterology Department, Loures, Portugal;(2)Mater Dei Hospital, Division of Gastroenterology, Msida, Malta;
Background
The early use of effective therapy may change outcomes in patients with Crohn's disease (CD). The aim of this study was to compare three different treatment strategies in CD (“top-down”, “accelerated step-up” and “regular step-up” therapy).
Methods
This was a retrospective multicentre study including patients with incident CD between 2009-2021. Patients were categorized into 3 treatment groups: group 1) “top-down”: anti-TNF ± immunomodulator (IM) within the first year of diagnosis with a maximum interval of 6 months between both drugs; group 2) “accelerated step-up”: IM within the first year of diagnosis followed by anti-TNF 6-12 months later, and group 3) “regular step-up”: IM within the first year of diagnosis with or without the need to further escalate to biologic (>12 months after the beginning of IM). The primary outcome was endoscopic healing (EH; SES-CD<3 and no ulcers) at the end of the follow-up; secondary outcomes were CD-related intestinal resection and hospitalization due to CD-flare. Cox regression analysis was performed and Kaplan-Meier curves were computed for each outcome.
Results
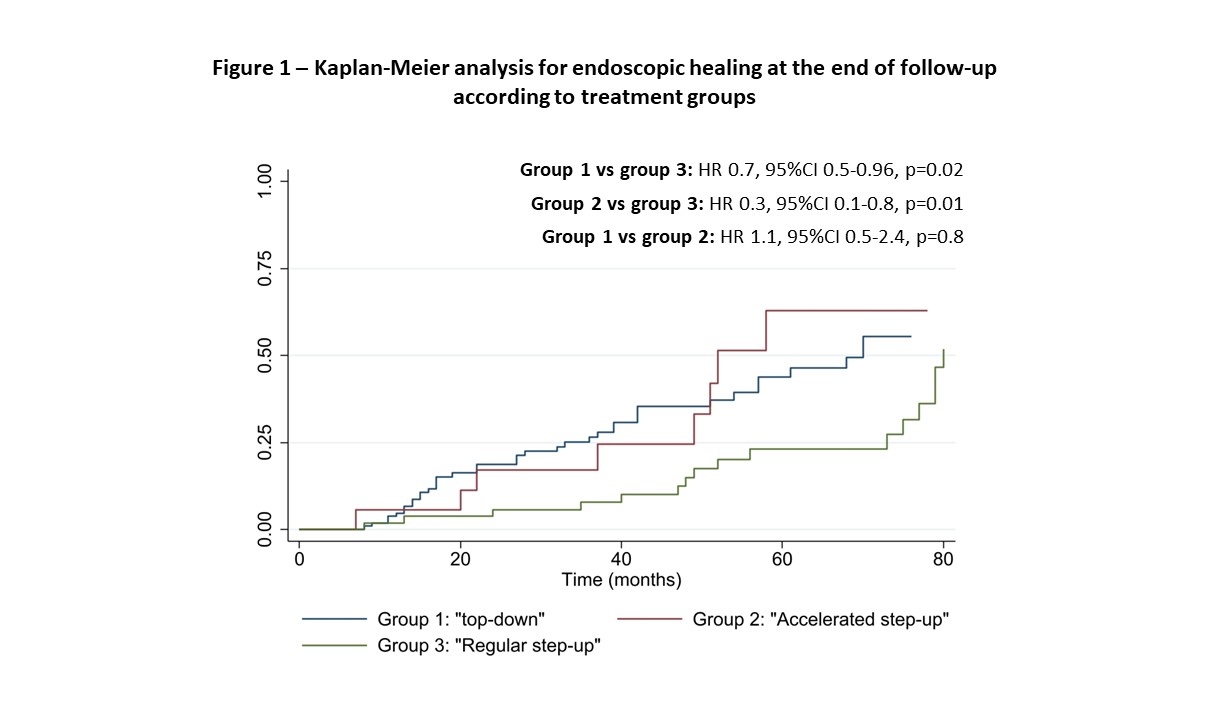
156 patients (54% males) were included, with 46% having ileocolonic disease (L3) and 68% an inflammatory phenotype (B1) at diagnosis. Baseline patients' characteristics in each different treatment strategy are demonstrated in Table 1. Patients were followed for a median of 69 (44-98) months; 12% in group 1 and 19% in group 2 had to switch biologicals (p=0.4); 64% in group 3 escalated to biologicals with a median time since diagnosis of 30 (20-50) months. In group 1, 73% of the patients used concomitant IM. At the end of follow-up, 50% of all patients achieved EH, 20% needed hospitalization and 13% had a CD-related intestinal resection. In a multivariate model adjusted for gender, age at diagnosis, disease location, disease behaviour, perianal disease, and prior surgery, patients in group 3 had a lower probability of achieving EH when compared with patients in group 1 (HR 0.7, 95%CI 0.5-0.96, p=0.02) and group 2 (HR 0.3, 95%CI 0.1-0.8, p=0.01). Kaplan-Meier curves are demonstrated in Figure 1. Using the same model, no differences were found in terms of hospitalization or need for intestinal surgery. Fistulizing disease was a significant predictor for intestinal surgery (HR 2.4, 95%CI 1.5-3.8, p<0.01).
Conclusion
Introduction of biological therapy within the first two years of diagnosis, either in a “top-down” or “accelerated step-up” approach was associated with a higher probability of achieving EH, as compared to the introduction of an immunomodulator followed by a later introduction of biologic. No differences were found for hospitalization or intestinal surgery. Fistulizing disease was a significant predictor for surgical intervention.


