P835 Visceral adiposity independently predicts time to flare in inflammatory bowel disease, but BMI does not
Sehgal, P.(1)*;Su, S.(2);Zech, J.(3);Nobel, Y.(1);Luk, L.(3);Economou, I.(4);Shen, B.(4);Kiran, P.(4);Freedberg, D.(1);
(1)Columbia University Irving Medical Center, Division of Digestive and Liver Diseases- Department of Medicine, New York, United States;(2)Columbia University Irving Medical Center, Department of Medicine, New York, United States;(3)Columbia University Irvine Medical Center, Department of Radiology, New York, United States;(4)Columbia University Irving Medical Center, Division of Colorectal Surgery- Department of Surgery, New York, United States;
Background
Obesity is rising globally and has been associated with increased IBD disease severity, prolonged hospital stay and increased development of extra-intestinal manifestations. Measuring “visceral adiposity” by CT scan may be a more meaningful way of classifying obesity compared to traditional measures such as BMI. This study compared visceral adiposity measured by CT scan versus BMI as a predictor of time to IBD flare among patients with CD and UC.
Methods
This was a retrospective cohort study. Consecutive adults with IBD were included if they had a colonoscopy to evaluate IBD flare and a CT scan within a 30-day window of the colonoscopy from 2010 to 2022. Charts were reviewed until 100 patients with Crohn’s and 100 with UC had been identified. Patients were followed for up to 6 months after the index CT scan for IBD flare, which was characterized by hospitalization/ER visit related to IBD, initiation of steroids, dose escalation, change in IBD medication, or IBD surgery. The primary exposure was the visceral adipose tissue to subcutaneous adipose tissue ratio (VAT:SAT) which was obtained from the index CT scan using TomoVision slicOmatic software. BMI was calculated based on height and weight at the time of the index CT scan. Cox proportional hazard modeling was used to test VAT:SAT and BMI as predictors of time to IBD flare, after adjusting for other factors.
Results
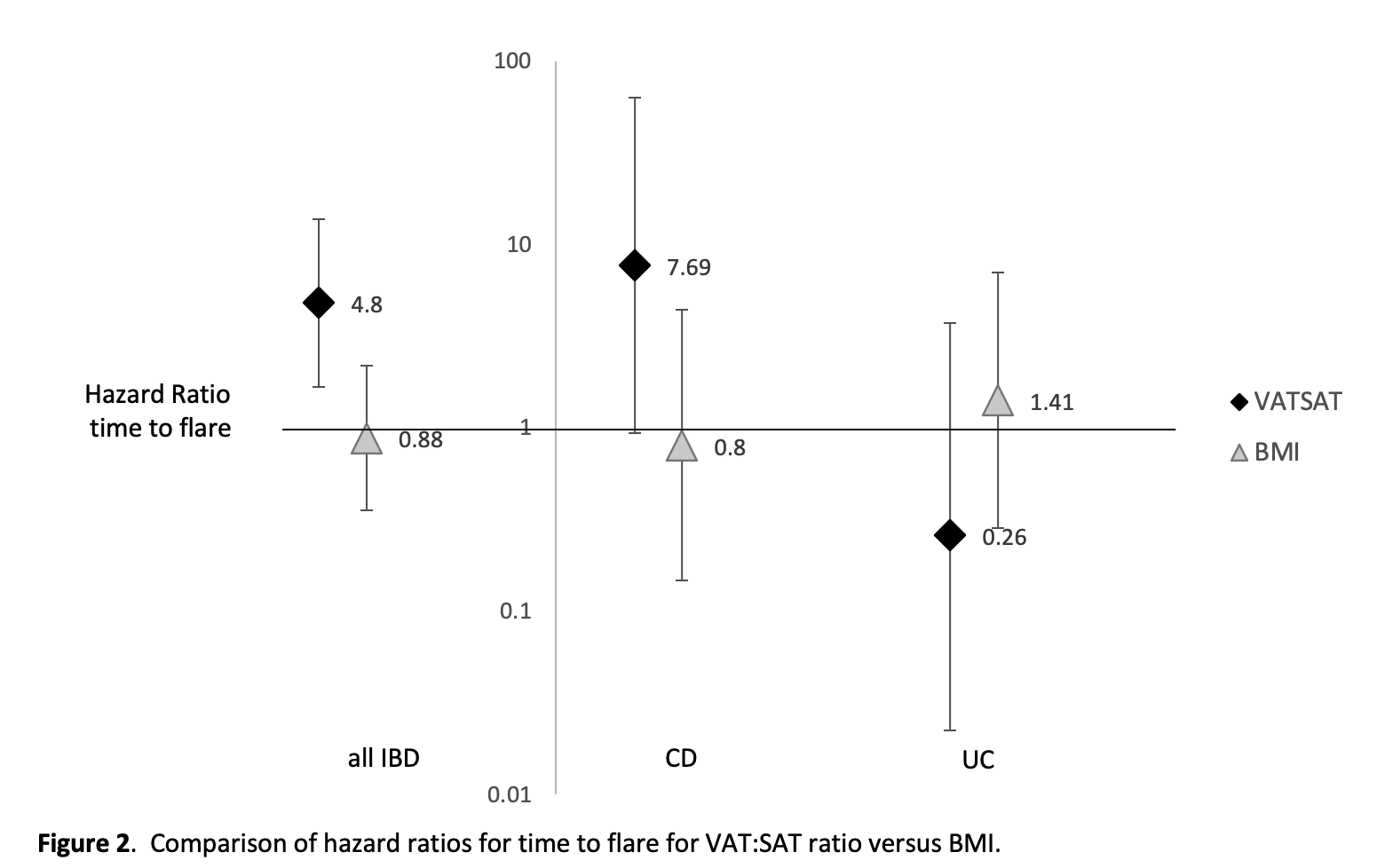
100 CD and 100 UC patients were included. The median age was 43 (IQR 31-58), 41% of the population was female, and most were White (55%) or Hispanic (26%). Overall, 20% of the cohort flared with a median time to flare of 88 days (IQR 42.5 – 118.5) among those who flared. For all patients, VAT:SAT was significantly associated with time to flare as seen in Figure 1 (HR 4.8, 95% CI 1.67 to 13.7 for VAT:SAT≥1.0 vs VAT:SAT<1.0), but BMI was not (HR 0.88 95% CI 0.35 to 2.18 for BMI ≥25 vs BMI <25). After stratifying the cohort into CD and UC cohorts, a significant association between VAT:SAT ≥1.0 and time to flare remained for CD (HR 7.68, 95% CI 0.93 – 63.2) but not for UC (HR 0.26, 95% CI 0.018 – 3.70). BMI was not associated with time to flare in either CD or in UC patients (Figure 2). 
Conclusion
Visceral adiposity (VAT:SAT ratio on CT scan) was associated with decreased time to IBD flare, but BMI was not. This relationship may be stronger among Crohn’s compared to Ulcerative colitis patients. Future studies should investigate the mechanisms by which visceral adiposity may contribute to IBD disease activity.


