P838 Increased Risk of Avascular Necrosis in Patients With Inflammatory Bowel Disease: a nationwide population based cohort study
Moon, J.M.(1)*;Kwon, K.E.(2);Jung, S.Y.(2);Choi, C.H.(1);Lee, J.W.(2);Shin, S.Y.(1);Joo, H.J.(1);
(1)Chung-Ang University College of Medicine, Department of Internal Medicine, Seoul, Korea- Republic Of;(2)Chung-Ang University, College of Pharmacy, Seoul, Korea- Republic Of;
Background
Avascular necrosis (AVN) is bone death due to disruption of blood supply causing disability and significant morbidity. Although considered multi-factorial, corticosteroid use is a well-known risk factor. Not only is AVN more prevalent in Inflammatory bowel disease (IBD), but IBD patients are often exposed to higher corticosteroids usage. Therefore, we aimed to investigate epidemiology and risk factors of avascular necrosis in Asian IBD patients.
Methods
We conducted a nationwide population-based cohort using Korean National Health Insurance Service (NHIS) database from January 2007 to December 2020. Newly diagnosed IBD patients were defined according to the International Classification of Diseases, 10th revision (ICD-10), and at least one prescription of IBD-specific medications. 1:3 sex-, age- matched subjects from the general population were selected. We investigated newly diagnosed AVN using the ICD-10 code and the incidence rates and risk of AVN were assessed with multivariate cox regression models.
Results
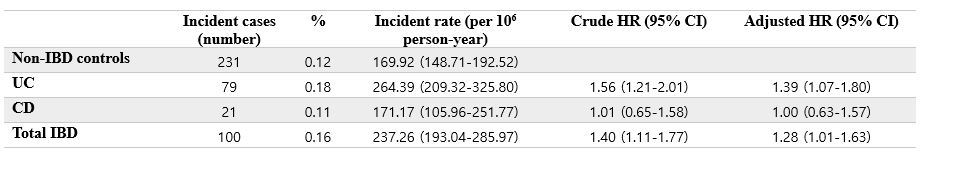
A total of 62,417 IBD population was identified, where ulcerative colitis (UC) comprised of 44,106. Age at diagnosis was younger in Crohn's disease (CD) than in UC (30±15 years and 43±16.3 years). UC population revealed greater number of comorbidities such as hypertension (16.7% and 7.1% for UC and CD, respectively), diabetes mellitus (12.4% and 9.5%), dyslipidemia (27.6% and 25.2%), and cerebrovascular diseases (4.5% and 2.5%). During the mean follow-up period of 6.75 years, 54,591 (87.5%) of the total IBD patients were exposed to systemic steroids (86.4% and 90.1% for UC and CD, respectively). Approximately 76.8% in the IBD group were prescribed with ≥10 mg/day of corticosteroids with mean duration of 16.3±35.1 days. A total of 100 (0.16%) newly diagnosed AVN cases were observed in the IBD population. Time from the index date to AVN diagnosis was 4.47±3.29 years. Compared to the non-IBD controls, the incidence of AVN was significantly increased in IBD subjects (adjusted hazard ratio [aHR] with 95% confidence interval [CI], 1.28 [1.01-1.63]). UC patients in particular were at an elevated risk for developing AVN (aHR with 95% CI, 1.39 [1.07-1.80]), whereas risk analysis for CD patients demonstrated results that were statistically not significant (aHR with 95% CI, 1.00 [0.63-1.57]).
Table 1 Incidence rates and risk ratios of AVN in patients with IBD
Conclusion
Risk of AVN was elevated in Korean IBD patients compared to non-IBD population, especially for UC. Physicians dealing with IBD patients should be aware of etiological factors of AVN along with corticosteroid use. Future study is needed to investigate on the mechanisms associated with AVN in IBD.