P846 Epidemiological and Clinical Characteristics of Inflammatory Bowel Diseases in Patients from Greece
Liava, C.(1)*;Sinakos, E.(1);Dimitroulas, T.(1);Navrozidou, C.(2);Akriviadis, E.(1,2);
(1)Aristotle University of Thessaloniki, Fourth Department of Internal Medicine- Hippokration General Hospital of Thessaloniki, Thessaloniki, Greece;(2)Interbalkan Medical Center of Thessaloniki, Gastroenterology Unit, Thessaloniki, Greece;
Background
There are few reports from Greece about the epidemiological and clinical features of inflammatory bowel diseases (IBD), which were mainly evaluated in retrospective studies with data collection from hospital registries. We aimed to determine the epidemiological profile and clinical features as well as to detect any differences between patients with Crohn’s disease (CD) and ulcerative colitis (UC), based on retrospectively-prospectively collected data from a cohort of IBD patients followed in daily clinical practice.
Methods
Patients with biopsy-confirmed IBD aged 10–90 years old were included in the study. A comprehensive questionnaire was used to collect data on each site visit from July 2018 until March 2022. Logistic regression analysis and chi-squared test were used to compare the frequency of epidemiological and clinical characteristics between patients with UC and CD.
Results
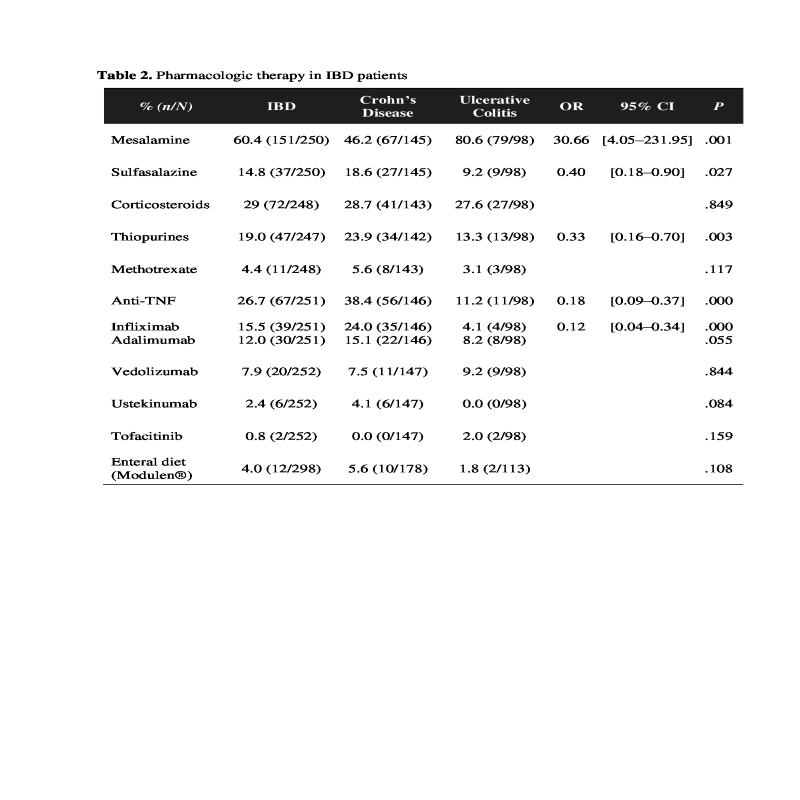
We collected 300 patients diagnosed with IBD (180 with CD, 113 with UC, and 7 with indeterminate colitis). The median age of IBD patients was 42 years. The onset of disease in CD group was observed between 17 and 40 years of age in the majority of patients (58%). Ileocolonic location of CD was present in 70% of CD patients; 39% had stricturing behavior and 29% had perianal disease (abscesses and fistulas). CD patients developed more often aphthous stomatitis (34%) than patients with UC (13%, OR 3.45; 95% CI: 1.76-6.78; P< .001). Patients with CD had a 20-fold increased risk to undergo a surgical procedure (OR 19.87; 95% CI: 6.03-65.48; P< .001), mainly enterectomy (26%), as shown in table 1. At study entry, C-reactive protein (CRP) elevation was more frequently present in CD compared to UC patients (OR 1.93; 95% CI: 1.04-3.59; P< .05). Most patients with UC had extensive colitis (56%). Mesalamine was predominantly used in UC patients (81% vs 46% in CD, P< .005), and sulfasalazine and thiopurines in CD patients (60-70% vs 9-13% in UC, P< .005), as shown in table 2. The most commonly used anti-TNF agent was Infliximab, mainly in CD patients (24% vs 4% in UC, OR 0.12; 95% CI: 0.04-0.34; P< .001). Adalimumab was used in 12% of IBD patients and Vedolizumab in 8%. Around 4% of patients with complicated CD received Ustekinumab. Tofacitinib was used in 2% of patients with severe complicated UC and extraintestinal manifestations. Enteral diet (Modulen®) was used in 6% of CD patients and in only 2% of UC patients with severe UC pancolitis.
Conclusion
In this retrospective-prospective cohort study of 300 patients with IBD, CD patients had a significantly higher risk of developing aphthous stomatitis and increased levels of CRP. CD patients also required more often treatment with anti-TNF agents and immunosuppressants, and a surgical procedure, mainly enterectomy.


