P859 Accuracy of self-reporting of immune-mediated inflammatory diseases by patients with inflammatory bowel disease. Results from a hospital-based cohort.
De Francisco Garcia, R.M.(1,2)*;Pérez-Martínez, I.(1,2);Castaño-García, A.(1);Celada-Sendino, M.(1);Fernández-González, E.(1);García-Pérez, C.(2);Martínez-Gozález, S.(2);Rolle, V.(2);Queiro, R.(3);Alonso-Castro, S.(3);Santos-Juanes, J.(4);Gueimonde, M.(2);Riestra, S.(1,2);
(1)Hospital Universitario Central de Asturias, Gastroenterology, Oviedo, Spain;(2)Instituto de Investigación Sanitaria del Principado de Asturias ISPA, Diet Microbiota and Health, Oviedo, Spain;(3)Hospital Universitario Central de Asturias, Rheumatology, Oviedo, Spain;(4)Hospital Universitario Central de Asturias, Dermatology, Oviedo, Spain;
Background
The association of several immune-mediated inflammatory diseases (IMIDs) in the same patient is well known. IMID, especially joint and cutaneous diseases, are frequently diagnosed in patients with inflammatory bowel disease (IBD). However, the degree of knowledge that patients with IBD have about the coexistence of other IMIDs is little studied. Our aim was to evaluate the accuracy of self-reporting of IMID by patients with IBD.
Methods
Prospective, unicentric study that included patients attended in person at the IBD Unit of the Central University Hospital of Asturias (Spain) between August 2020 and December 2021. Patients were invited to participate in the study, and, after signing the informed consent, they answered a questionnaire about the presence or not of 50 IMIDs (self-reported diagnosis). The diagnosis of an IMID was confirmed in the medical records of each patient (reference diagnosis). Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy (proportion of subjects correctly classified) of self-reporting was calculated. Statistical analyses were performed with R software version 4.0.2.
Results
A total of 1,621 patients were included. Forty-four percent of patients had ulcerative colitis, 53% had Crohn's disease and 3% had an IBD-unclassified, 50% were men, and the age at diagnosis of IBD was 38±15.2 years. Seven hundred and twelve patients were receiving mesalazine, 67 corticosteroids, 394 immunomodulators and 532 biologics. Six hundred and twenty-seven (39%) patients were diagnosed with at least one IMID, 177 (10.9%) with two, 49 (3%) with three, and 17 (1%) with more than three. Sixteen percent of patients had a joint IMID and 15% a cutaneous IMID. Self-reporting of IMID by IBD patients has a sensitivity, specificity, PPV, NPV and accuracy of 0.75 (95% CI 0.73-0,78), 0.89 (95% CI 0.86-0.91), 0.92 (95% CI 0.89-0.93), 0.69 (95% CI 0.66-0.73) and 0.81 (95% CI 0.79-0.83), respectively. Table 1 shows the results by IMID groups (joint, cutaneous, digestive, endocrinological, ocular, others), and Table 2 shows the results of the most frequent IMIDs.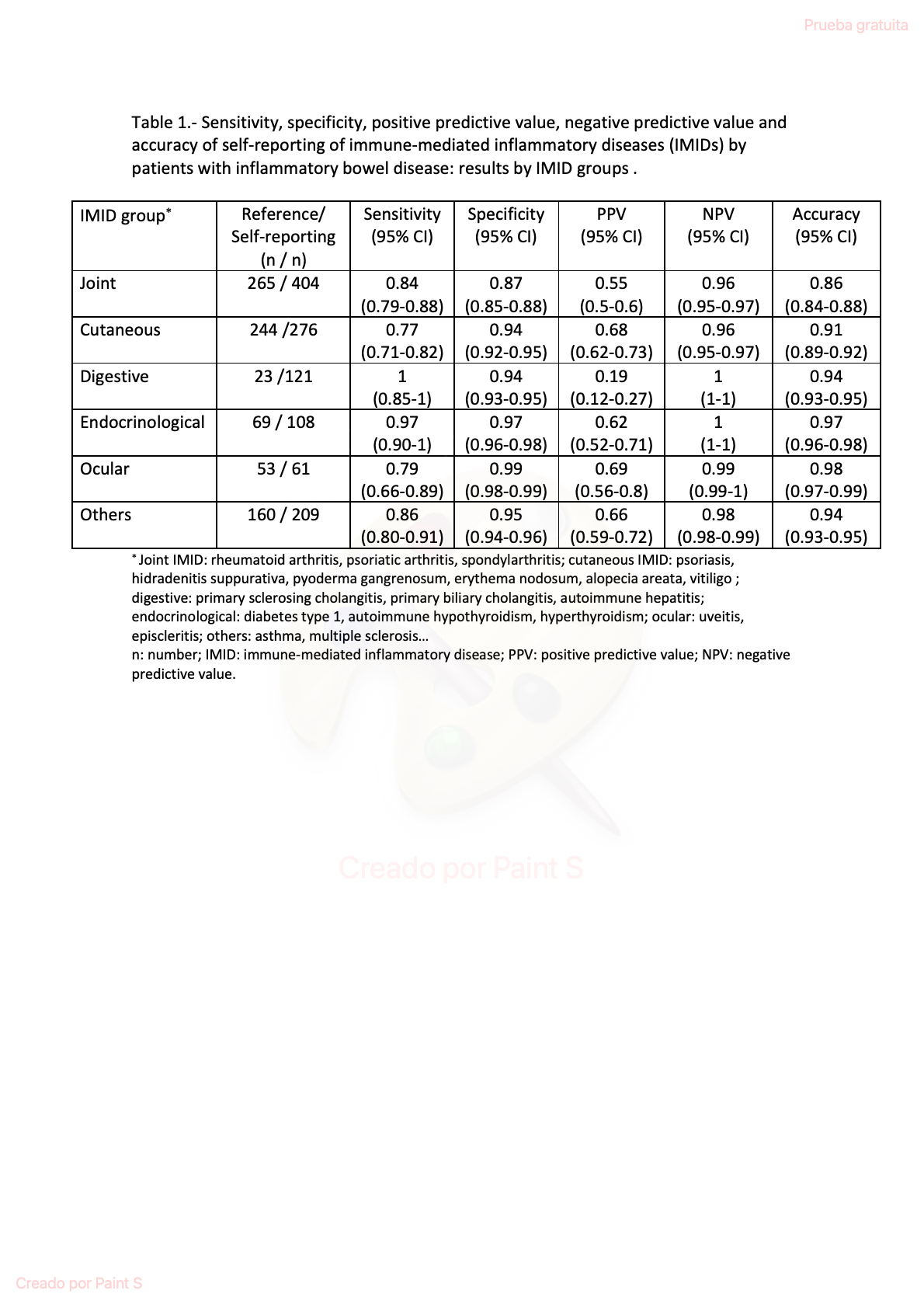

Conclusion
Eighty-one percent of patients with IBD are able to correctly identify the coexistence or not of IMIDs. It was observed that in the case of joint IMIDs there is a significant percentage of patients who do not know whether or not they suffer from one of these diseases.


