Diet in the management of IBD: Current status and future perspectives
This Symposium was sponsored by Nestlé Health Science
 |
Introduction to Diets in the Management of IBD
Prof. Franck Carbonnel
Professor of Gastroenterology, University Paris Sud, France
Head, Gastroenterology Department, University Hospital of Kremlin Bicetre, Paris, France
In recent years, studies have shown the associations between food and the risks of developing Inflammatory Bowel Disease (IBD).
An early study showed a significant link between the consumption of red meat and the likelihood of developing Ulcerative Colitis (UC). Subsequent studies deepened our knowledge, pointing to associations between UC and a high consumption of omega-6, and low consumption of omega-3, fiber (fruit and vegetables), zinc and potassium.1,2,3,4,5,6,7,8,9
Other studies have shown a decreased risk of Crohn’s Disease (CD) in people who consume a larger proportion of unprocessed or minimally processed food, and an association between proinflammatory diets, ultra-processed foods, non-Mediterranean diet and CD.1-8,10,11,12,13,14
This set of work has paved the way towards a new question: Can IBD be treated with diets? Recent studies15,16,17,18,19 have providedevidence that this could be the case. Alongside other diets, the Crohn’s Disease Exclusion Diet (CDED) has been shown in an RCT and through real-world clinical evidence to be effective in inducing remission in children with mild to moderate CD, and may support maintenance of remission.20
There is also emerging evidence of the effectiveness of CDED in adults.21,22 To further consolidate these findings a new multicentric RCT, the PARADISE study, has been initiated to explore CDED+PEN vs prednisone for induction of remission in adult CD patients.
Diets for the management of IBD: Where we stand and future perspectives
Eytan Wine, MD, PhD, FRCPC
Professor of Pediatrics and Physiology, University of Alberta, Canada
A 2019 randomized control study, first presented at ECCO, has helped to establish the general principles of the CDED.23
General principles of CDED:
- Exclusion of foods known to affect the host health and/or microbiota
- Inclusion of foods known to promote rebiosis
- A balanced diet to ensure patient nutritional health
- A progressive diet to promote palatability and acceptance
Initial studies examining the efficacy of CDED
In a 12-week prospective trial of children with mild to moderate CD conducted in 20191, children were randomly assigned to a group that received CDED plus 50% of calories from partial enteral nutrition (PEN, Modulen IBD) for 6 weeks (phase 1), followed by CDED with 25% PEN from weeks 7 to 12 (phase 2).
The study showed that CDED plus PEN was better tolerated than exclusive enteral nutrition (EEN) in children with mild to moderate CD. The combination of CDED plus PEN induced sustained remission in a significantly higher proportion of patients than EEN and produced changes in the fecal microbiome associated with remission.
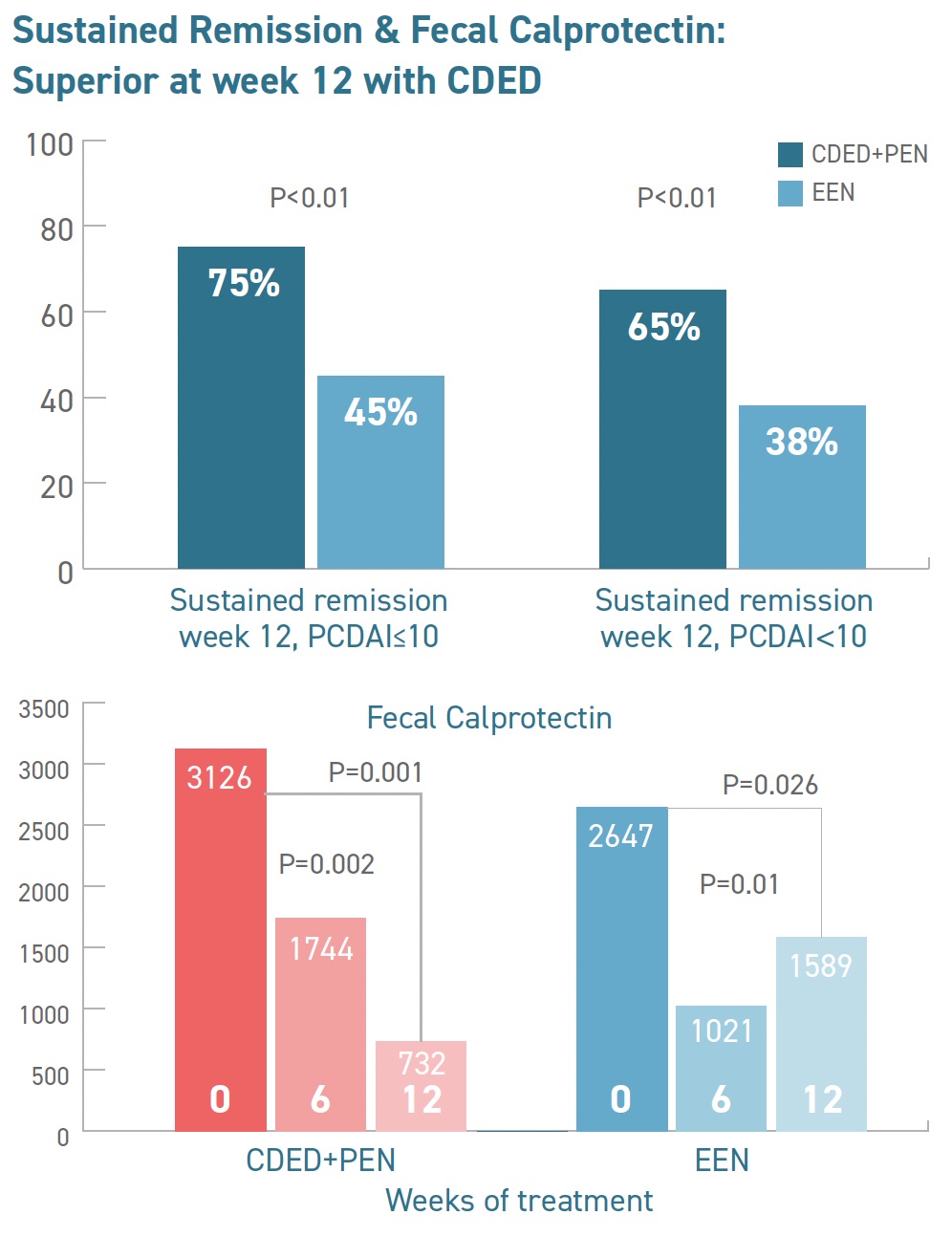
Figure 1.
Following this study, a number of reports confirmed the effectiveness of CDED+PEN in practice, making CDED a well-recognized and important alternative to EEN.
The next stage was to investigate whether CDED can be used to treat adults with CD, patients with severe luminal CD, therapy for longer than 12 weeks and for patients refractory to biologics and/or as an adjuvant therapy to biologics.
Studies that support the use of CDED in treating adults with CD
A 2021 prospective study in adults24 treated 32 patients with mild to severe CD. Patients were seen at baseline, at week 6, and at week 12. At week 6 there was a 76.7% clinical remission rate. Remission rose to 82.1% at 12 weeks.
In another randomized controlled trial25, 44 adults with mild to moderate CD were treated with CDED. Patients were randomly assigned to CDED plus PEN (20) or CDED alone (24) for 24 weeks. The primary endpoint was clinical remission.
At week 6, 68.4% of patients in the CDED plus PEN group and 57.1% of patients in the CDED alone group had achieved clinical remission (p=0.4618). Among the 25 patients in remission at week 6, 63.2% and 38.2% were in sustained remission at week 24 in the CDED+PEN and the CDED alone group respectively. 35% of the overall patient cohort were in endoscopic remission at week 24.
The implications of current studies
Compared to other available therapies, these results were very encouraging. As a result, guidelines set by the European Society for Clinical Nutrition and Metabolism (ESPEN)26 recommend that: “CD exclusion diet (plus partial EN) should be considered as an alternative to exclusive EN in pediatric patients with mild to moderate CD to achieve remission.” For adults, a lower grade recommendation suggests that: “A CD exclusion diet can be considered with or without EN in mild to moderate active CD.” The expert panel commented that this should be further demonstrated with additional studies.
Conclusions
CDED is now the best documented effective dietary therapy (besides EEN) in inducing remission in CD. There is increasingly new data on CDED use in adults and those with more severe CD. The next step is to look for new indications for using CDED, including in combination with other therapies, and exploring new ways to improve CDED success for pediatric IBD patients.
Practical cases of using CDED in adult patients
Catherine Westoby, RD, MRes
Gastroenterology & Research Dietitian, University Hospital Southampton NHS Foundation Trust, UK
There is an unmet need for severe Crohn’s Disease patients beyond the current EEN proposition. In the case studies presented, we share our practical experience in using CDED in adults with refractory disease, as an adjunctive therapy, or in patients experiencing loss of response to biologics, for induction and maintenance of remission.
Case study 1: Loss of response to biologics
A 22-year-old female (70 kg, BMI, 27 kg/m2) presented with symptoms of abdominal pain, diarrhea and vomiting.
MRI showed 5–10 cm patchy ileocecal inflammation (ICV). Colonoscopy showed deep ulcers in ICV. The patient had previously demonstrated loss of response to infliximab, adalimumab and azathioprine, and was being treated with ustekinumab weekly.
The patient was reloaded with ustekinumab and reduced from 8 to 6 weekly; however, fecal calprotectin (FC) continued to rise (2094 μg/g). She was then referred for EEN.
Initial assessment
Following a difficult experience with EEN as a child, the patient was unwilling to go back on EEN.
Plan for phase 1: CDED with 50% of requirements met with 200 g Modulen IBD.
Six-week review
FC reduced to 1616 μg/g.
Plan for phase 2: continuation of CDED and 100 g Modulen (25% of EN requirement).
14-week review
FC further reduced to 194 μg/g (week 12.5).
The patient reported feeling unwell (likely due to obstructive episodes). The decision was made to move to a liquid only diet (400 g Modulen) until symptoms settled, followed by softer texture food from phase 1 and 2 diets to reduce obstruction risk and symptoms.
FC 178 μg/g (week 18).
Repeat MRI and dietetic review, October 2020
MRI showed a reduction in abnormality from 2019. The patient only required EEN for two days, had gained 4.6 kg since CDED, had managed well on phase 2 and moved to phase 3, was passing formed motions and did not require surgery.
Current update
The patient remained in remission for 27 months between April 2020 and July 2022. After a short period without Modulen and eating a free diet whilst overseas, the patient experienced a severe flare and obstruction in September 2022. The patient regained more control symptomatically by going on 6 weeks of EEN in addition to steroids and is now on phase 2 CDED+PEN (Modulen) again.
Case study 2: Complex fistulating disease
A patient with complex fistulating disease with marked pre-stenotic dilatation in multiple sites throughout the small bowel was weened onto EEN for 1 week followed by CDED phase 1, 2 and 3 successfully following a period of bowel rest with parenteral nutrition. He regained response to biologics and managed to avoid surgery, regained the weight he had lost (37 kg in 14 months) and remained on 25% requirements as partial enteral nutrition (PEN) and CDED maintenance diet long term due to complex disease.
Case study 3: Postoperative ileostomy
A patient with an ileostomy was referred for CDED postoperatively to reduce his risk of postoperative recurrence as he was at risk of short bowel syndrome if he required further surgery and had failed multiple drug therapies.
Following 2 weeks of EEN he was successfully weened onto CDED phase 1, 2 and 3, respectively, with dietetic adaptations and close monitoring due to his more complex disease. He did not tolerate apples so was advised to exclude them and have the alternative allowed fruit. He was also advised to avoid the beans and whole nuts in phase two to limit obstruction risk. He tolerated the diet very well with no increase in stomal losses despite eating more fruit and vegetables than he had in previous years and he remains in remission 2.5 years later.
Conclusions and dietetic considerations
CDED is a useful treatment for Crohn’s Disease, including complex disease phenotypes with careful dietetic adaptations. Considerations when commencing patients on CDED are that they will require 6 weekly dietetic reviews initially, or more frequently than this in more complex cases. Calcium intake and the potential need for additional supplementation should be considered, particularly in patients who do not drink an adequate volume of PEN. In patients who are malnourished or who have stricturing disease, a higher proportion of PEN may be temporarily required over and above the usual recommendation of 50% of energy requirements in phase 1 to promote weight gain or reduce the risk of obstruction, respectively. The collection of outcomes such as FC, CRP and validated tools such as Harvey Bradshaw and IBD control are useful to evaluate the success of the CDED as a therapeutic diet.
Patient selection for CDED is important. For complex fistulating disease, EEN would still be the first line, but CDED can be considered if the patient is stable enough without the presence of abscesses, usually after an initial period of EEN. If a patient presents with tight inflammatory strictures or a bowel obstruction, EEN would also be considered as the first line. However, with small adaptions, CDED can still be used once inflammation reduces.
The return of symptoms during the maintenance phase can pose a challenge; however, this can often be related to the level of patient compliance and can be managed by a careful dietetic follow-up.
Food diversity offered within CDED is particularly well appreciated by patients and provides motivation for complying with the treatment. Access to support material and multiple recipes through the Modulife App is an asset for patients, and the latter reduce monotony.
New perspectives in dietary management of Ulcerative Colitis
Chen Sarbagili-Shabat, Msc RD
Registered Dietitian & Researcher, Wolfson Medical Center, Tel Aviv Sourasky Medical Center, Tel Aviv University, Israel
Dietary management of CD has been documented, but we know that what works for CD does not necessarily work for UC.27
The principles of UCED are to reduce or exclude certain dietary components that have been shown to have a negative effect on the microbiome–host interaction through several mechanisms: barrier function, mucosal immunity, colonic metabolites, and energy homeostasis. These include sulfated amino acids, dietary sulfur, processed foods, animal protein and saturated fat.
The diet emphasizes components that offer a protective effect, including fruit and vegetable fibers, pectin and resistant starch, and tryptophan. UCED has some important distinctions from the CDED:
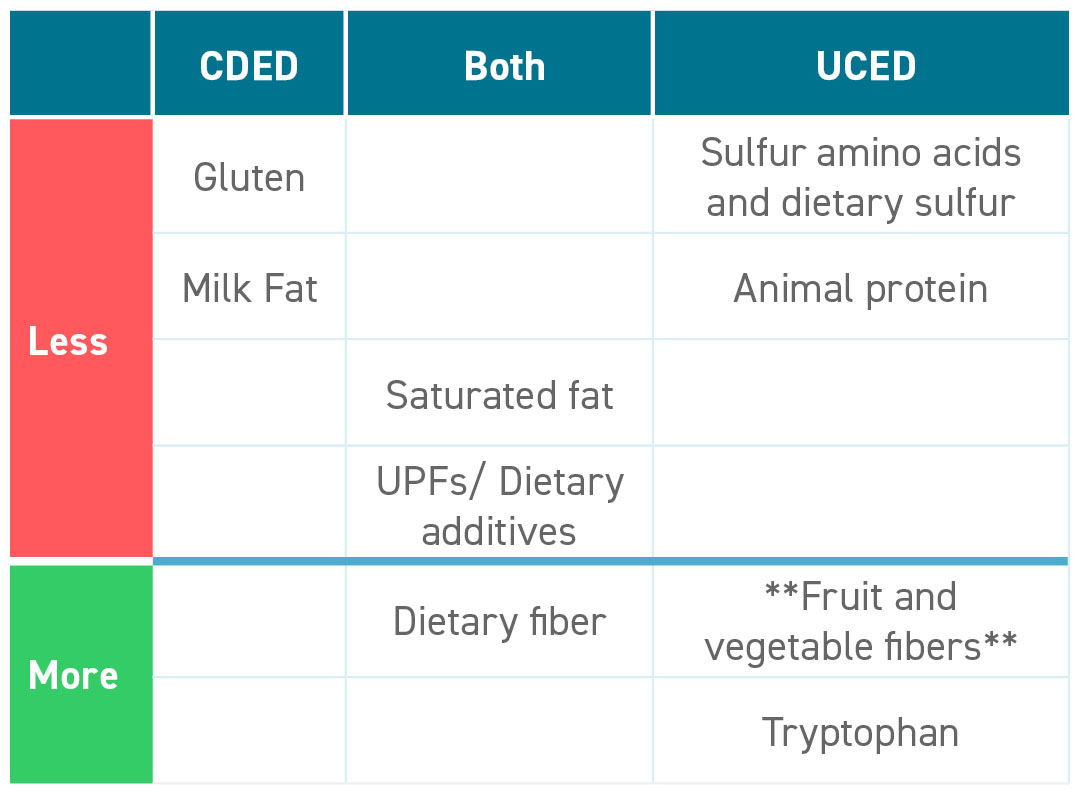
Figure 2.
Studies are now underway to establish if an Ulcerative Colitis Exclusion Diet (UCED) could provide a treatment option for UC patients.
A first study28 was conducted in adult patients with clinical endoscopic disease (29% steroid-refractory patients, 55% biologic-refractory patients). Patients were randomized to one of three groups:
- Group 1 received a free diet and a single donor standard fecal transplant (FT) by colonoscopy on day 1 and rectal enemas on days 2 and 14 without dietary conditioning of the donor.
- Group 2 received FT as above but with dietary preconditioning of the donor for 14 days and a UCED for the patients.
- Group 3 received the UCED alone.
Primary endpoint: clinical steroid-free remission (SCCAI <3) at week 8.
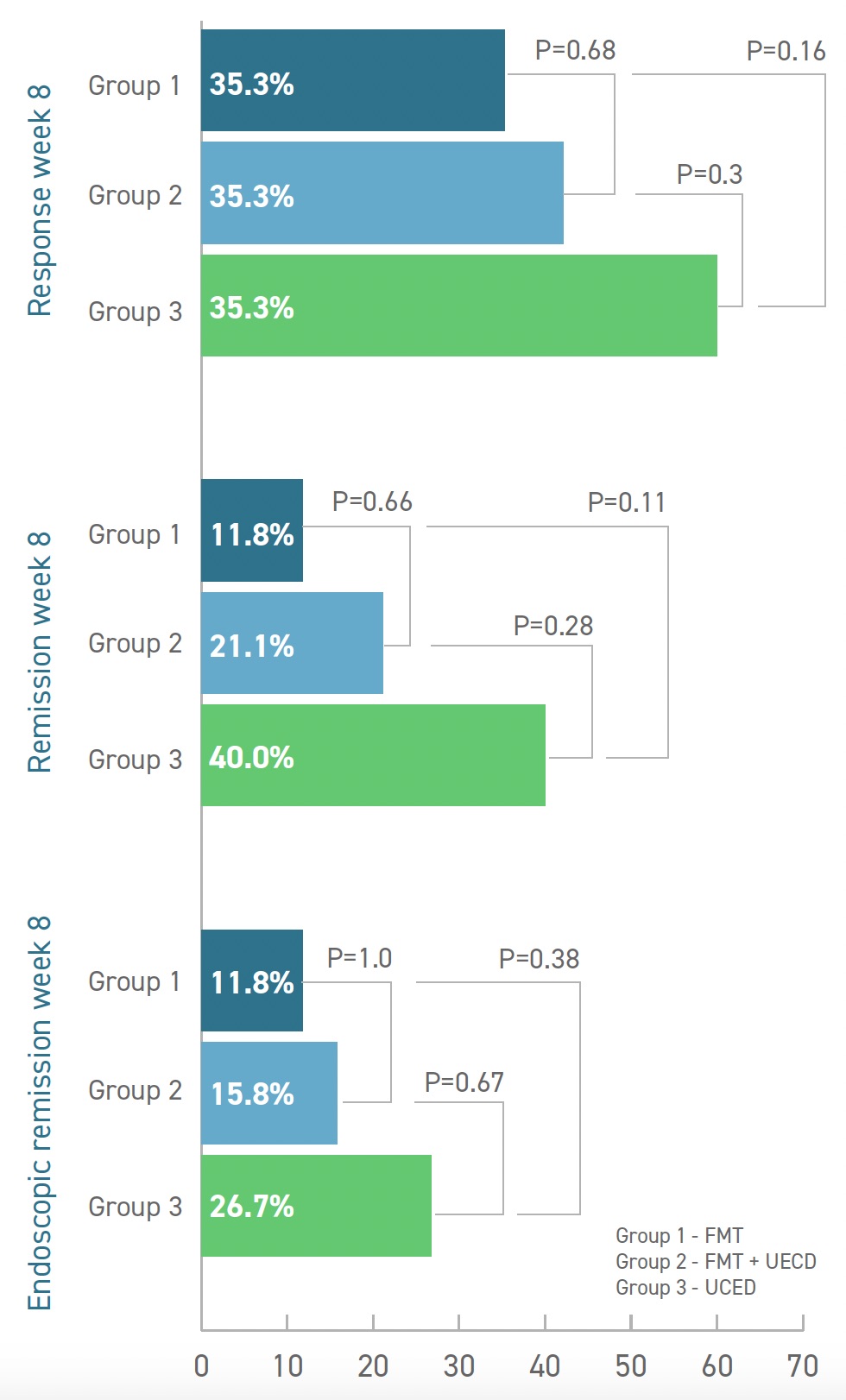
Figure 3.
Group 3 (UCED alone) showed the highest rate of clinical remission (40%) and endoscopic remission (27%). Group 3 also demonstrated a significant decrease in the Simple Clinical Colitis Activity Index (SCCAI) at week 8. A significant proportion of patients worsened after FT (Group 1 or Group 2) by week 8 compared to baseline. Group 3 reported the least worsening of disease.
None of the therapies were effective for the most severe patients (SCCAI >9). Only one out of 28 biologic refractory patients achieved clinical remission.
A second study looked at the effect of UCED in pediatric patients with mild-to-moderate active disease.29 Patients were introduced to UCED for the first 6 weeks, and those in remission at week 6 received a step-down diet for another 6 weeks.
Median Pediatric Ulcerative Colitis Activity Index (PUCAI) decreased from a baseline of 35 (30–40) to 12.5 (5–30) at week 6 (p=0.001).
Among five patients who achieved remission at week 6, median FC level decreased from 630 (IQR 332–1586) μg/g to 230 (75–1298) μg/g (p=0.14).
71% of patients achieved clinical response and 38% achieved clinical remission. An improvement in FC was also seen after dietary intervention.
UCED clinical outcomes: adult vs pediatric
Clinical outcomes were consistent in adults and children. 60% of adults achieved clinical response vs 71% of children. 40% of adults and 38% of children achieved clinical remission.
Following the studies, it was felt that UCED combined with PEN would provide complementary nutritional support and improve outcomes.
Currently a new multicenter RCT (ReDUCE) is aiming to evaluate if UCED plus PEN can improve outcomes when administered with an oral budesonide regimen to adults with mild to moderate UC.
The rationale behind using UCED with PEN is: to support dietary intake with an oral liquid formula (pilot studies showed a decreased energy intake), to provide balance of micro- and macronutrients, to increase adherence and efficacy, to help deliver optimal fiber, and to help personalize recommendations.
After randomization patients can enter one of two groups:
- Group 1: UCED + PEN
- Group 2: Control group on free diet
Both groups will receive 9 mg oral budesonide. Primary endpoint: remission at week 12. Where CDED + PEN studies used Modulen, in the new UCED + PEN study, a novel specifically designed formula in compliance with the UCED will be used.
Conclusions
Studies indicate differences in the dietary effect and mechanism of action between UC and CD. UCED positively affects clinical and endoscopic outcomes, and appears to be a promising approach for the induction of clinical remission and endoscopic remission in the milder spectrum of refractory disease. However, further trials are required before clinical application.
Final comments from the panel
Fibre may play a more complex role in IBD than previously recognised. Current data suggest that the response to fibre is influenced by diet, microbes, the gut barrier, immune cells and active inflammation.
The key message should remain that fibres are good for gut health and most patients should be consuming fibre. However, caution should still be made in advising fibre as different types of fibre may have different impacts on microbiota and inflammatory response.
References
1 Dong C, et al. Meat intake is associated with a higher risk of ulcerative colitis in a large European prospective cohort study. J Crohns Colitis. 2022 Aug 30;16(8):1187-1196.
2 D Chan, et al. Inflammatory bowel disease and exercise: results of a Crohn's and Colitis UK survey. Frontline Gastroenterol. 2014 Jan;5(1):44-48.
3 Tjonneland A, et al. Linoleic acid, a dietary n-6 polyunsaturated fatty acid, and the aetiology of ulcerative colitis: a nested case-control study within a European prospective cohort study. Gut. 2009 Dec;58(12):1606-11.
4 Andersen V, et al. Fibre intake and the development of inflammatory bowel disease: A European prospective multi-centre cohort study (EPIC-IBD). J Crohns Colitis. 2018 Jan 24;12(2):129-136.
5 Ananthakrishnan A, et al. Long-term intake of dietary fat and risk of ulcerative colitis and Crohn's disease. Gut. 2014 May;63(5):776-84.
6 Ananthakrishnan A, et al. A prospective study of long-term intake of dietary fiber and risk of Crohn's disease and ulcerative colitis. Gastroenterology. 2013 Nov;145(5):970-7.
7 Ananthakrishnan A, et al. Zinc intake and risk of Crohn’s disease and ulcerative colitis: a prospective cohort study. Int J Epidemiol. 2015 Dec;44(6):1995-2005.
8 Khalili, et al. Identification and characterization of a novel association between dietary potassium and risk of Crohn's disease and ulcerative colitis. Front Immunol. 2016 Dec 7;7:554.
9 Dugelay E, et al. Dietary zinc intake and inflammatory bowel disease in the French NutriNet-Santé cohort. Am J Gastroenterol. 2020 Aug;115(8):1293-1297.
10 Lo C, et al. Dietary inflammatory potential and risk of Crohn's disease and ulcerative colitis. Gastroenterology. 2020 Sep;159(3):873-883.e1.
11 Racine A, et al. Dietary patterns and risk of inflammatory bowel disease in Europe: Results from the EPIC Study. Inflamm Bowel Dis. 2016 Feb;22(2):345-54.
12 Vasseur P, et al. Dietary Patterns, Ultra-processed food, and the risk of inflammatory bowel diseases in the NutriNet-Santé cohort. Inflamm Bowel Dis. 2021 Jan 1;27(1):65-73.
13 Narula N, et al. Association of ultra-processed food intake with risk of inflammatory bowel disease: prospective cohort study. BMJ. 2021 Jul 14;374:n1554.
14 Khalili H, et al. Adherence to a Mediterranean diet is associated with a lower risk of later-onset Crohn's disease: results from two large prospective cohort studies. Gut. 2020 Sep;69(9):1637-1644.
15 Levine et al., Crohn’s Disease Exclusion Diet plus partial enteral nutrition induces sustained remission in a randomized controlled trial. Gastroenterology. 2019;157:440-450
16 Sigall-boneh et al., Dietary therapies induce rapid response and remission in pediatric patients with active Crohn’s disease. Clin Gastroenterol Hepatol. 2021 Apr 1, Vol. 19, Issue 4, p.752-759.
17 Niseteo et al., Modified Crohn’s disease exclusion diet is equally effective as exclusive enteral nutrition: Real-world data. Nutr Clin Pract. 2021;1-7.
18 Scarallo L et al., Crohn’s Disease Exclusion Diet in children with Crohn’s disease: a case series. CMRO. 2021, Volume 37, Issue 5.
19 Matuszczyk et al., Effect of the Crohn’s Disease Exclusion Diet (CDED) on the fecal calprotectin level in children with active Crohn’s disease. J Clin Med. 2022, 11, 4146
20 Fitzpatrick J, Melton S, et al. Dietary management of adults with IBD - the emerging role of dietary therapy. Nat Rev Gastroenterol Hepatol. 2022 Oct;19(10):652-669.
21 Szczubelek et al, Effectiveness of Crohn’s disease exclusion diet for induction of remission in Crohn’s disease adult patients. Nutrients. 2021;12:4112.
22 Yanai et al., The Crohn’s disease exclusion diet for induction and maintenance of remission in adults with mild-to- moderate Crohn’s disease (CDED-AD): an open-label, pilot, randomized trial. Lancet Gastroenterol Hepatol. 2022;7:49-59.
23 Levine A, Wine E, et al. Crohn's Disease Exclusion Diet plus partial enteral nutrition induces sustained remission in a randomized controlled trial. Gastroenterology. 2019 Aug;157(2):440-450.e8.
24 M Szczubełek, Pomorska K, et al. Effectiveness of Crohn’s Disease Exclusion Diet for induction of remission in Crohn’s disease adult patients. Nutrients. 2021 Nov 17;13(11):4112.
25 Yanai H, Levine A, et al. The Crohn’s Disease Exclusion Diet for induction and maintenance of remission in adults with mild-to-moderate Crohn’s disease (CDED-AD). Lancet Gastroenterol Hepatol. 2022 Jan;7(1):49-59.
26 Bischoff S, Bager P, et al. ESPEN guideline on clinical nutrition in inflammatory bowel disease. Clinical Nutrition. 2023 March; 42(3) 352-379.
27 Nikolaus S, Schreiber S. Diagnostics of inflammatory bowel disease. Gastroenterology. 2007 Nov; 133(5):1670-89.
28 Sarbagili Shabat C, Scaldaferri F. Use of faecal transplantation with a novel diet for mild to moderate active ulcerative colitis: The CRAFT UC Randomised Controlled Trial. J Crohns Colitis. 2022 Mar 14;16(3):369-378.
29 Sarbagili Shabat C, Scaldaferri F. A Novel UC exclusion diet and antibiotics for treatment of mild to moderate pediatric ulcerative colitis: A prospective open-label pilot study. Nutrients. 2021 Nov; 13(11): 3736.
Disclaimer: This programme is not affiliated with ECCO.


